Key points
- The NHS is emerging from the greatest challenge it has faced. Despite fears that it would be overwhelmed, the NHS has innovated and adapted not only to manage a huge wave of COVID-19 patients, but also to continue to treat millions of patients not infected with the virus and to roll out its largest ever vaccination programme.
- The scale of innovation seen in the NHS has been a defining feature of the pandemic. Staff have been redeployed, patient services have been delivered in new ways, there has been greater use of digital technology for clinical purposes, and local organisations have enhanced the way they work together. These will be essential ingredients if the NHS is to become an even higher performing system.
- But the last year has come at a considerable cost to health and care staff and local communities, not least when it comes to exacerbating health inequalities. NHS leaders know the service must play its role in addressing systemic inequality, unfairness and injustice. As part of this, NHS leaders want to make sure inequalities are not widened as they address the backlog of care. This will require, as one NHS leader told us, a ‘generational change’ in our approach.
- The pandemic will leave a backlog of care in excess of anything we have seen over the last decade. As well as more people waiting, people are waiting longer. The waiting list is now at 5.61 million and there is a 'hidden' waiting list of more than 7 million. A key focus will be finding the 'missing’ 7 million, as we know many of them will be from deprived and marginalised groups. There are already indications that waiting lists have grown more rapidly in more deprived areas during the pandemic. The NHS is based on the founding principles of care being free at the point of use, on the basis of need and not ability to pay. For the NHS to live up to its founding principles, we need a new approach to dealing with the backlog that is based on targeting those in most need, and not solely responding to demand for care from those who come forward.
- Throughout the summer, NHS leaders in England have said their organisations are experiencing winter levels of demand. NHS acute, mental health, community, ambulance and primary care services are all seeing more patients seeking urgent care and more with complex needs. And we are facing a pandemic of mental illness. The complexity of care, threat from new COVID-19 variants, and the need to operate with infection prevention and control measures will hamper productivity for months to come and make it harder to address the backlog. The pressures felt across all parts of the system can only be overcome by working in a truly integrated way.
- Our staff are our key asset, but many are exhausted. NHS leaders say that understaffing is putting patient safety and care at risk, and many are concerned about the long-term impact of COVID-19 on the wellbeing of their staff. We know that many staff are at the edge of retirement, and after 18 months of sustained pressure, if we push staff too hard, we may lose them. They want to see sustained government action to address the more than 93,000 NHS vacancies, as well as providing ongoing support for staff health and wellbeing. We are also working to ensure that our commitment to educating our future professionals is honoured in light of the contribution that undergraduate and postgraduate students made to the pandemic response.
- At the same time as addressing the care backlog and COVID-19, the English NHS is being reformed, with the government having now published draft legislation that will boost efforts to integrate care. These reforms are widely supported, but NHS leaders face a huge challenge in getting integrated care systems (ICSs) ready to become statutory organisations by April 2022. NHS leaders must be supported so that they can get on with the real purpose of the reforms: putting population health strategies centre stage and delivering effective integration across the NHS and social care so they can tackle worsening health inequalities.
- With multiple challenges ahead, NHS leaders have been calling for funding certainty. This partially came on 7 September when the government announced welcome extra funding for the NHS and social care. This will help the NHS make a start on tackling backlogs, but it has not gone far enough. As our report with NHS Providers shows, the NHS needs £10 billion next year, not the £6.5-7 billion that it will get. And the government’s funding is predicated on the assumption that COVID-19 infection rates will be low in 2022 and beyond.
- There will now have to be difficult decisions between the demands of elective recovery, mental health and staff wellbeing, and the generational task of reducing health inequalities. This will require political leadership to help manage public expectations about the recovery task ahead. And it will require the government to reorient resources towards long-term investment in public health, population health management and reducing the long-standing health inequalities that we know have contributed to the levels of infection, harm and death due to COVID-19 in poorer and ethnic minority communities.

This report sets out the views of healthcare leaders in England on the measures needed to ensure the NHS can meet the key challenges it faces, including addressing the backlog of care and health inequalities that have been exacerbated by COVID-19. It also explores how the health and care sector can sustain the beneficial changes that have resulted from the pandemic.
Introduction
Since April 2020, we have been convening our members – leaders from across the health systems of England, Wales and Northern Ireland – along with our partners and national leaders working in government and the arm’s-length bodies, to reflect on the learning from the pandemic and what it means for the future of health and care.
As part of our NHS Reset campaign, over the course of nearly 100 webinars, roundtables and private meetings with more than 3,000 leaders, we have explored the shifts in ways of working, culture, regulation, assurance and behaviour that have accompanied the response to COVID-19.
This report is the latest in our NHS Reset series. It sets out the views of healthcare leaders in England on the changes that are required as the NHS attempts to tackle a huge backlog of care and widening inequalities.
The centrepiece of the report is a survey of the NHS Confederation’s Health Leaders Panel. This is the only panel of its kind in the health sector in England. It comprises 100 leaders from across the whole healthcare system, including:
- chairs and chief executives of acute, community, mental health and ambulance provider trusts, as well as voluntary sector providers
- chairs and executive leads of integrated care systems
- clinical directors and managers of primary care networks and chief executives of primary care federations
- chairs and accountable officers of clinical commissioning groups.
For this latest report, we surveyed members of the panel during July 2021. In partnership with NHS Providers in August, we also surveyed hospital, mental health, community and ambulance service trust chief executives to examine their expected cost pressures in 2022.
Charting a new course
It is clear from our survey and the engagement we have had with healthcare leaders in recent months that several key issues need to define the next stage of the health and care system’s recovery from COVID-19 and its future development. These factors are explored in detail in the next section of the report.
A sustained focus on tackling health inequalities
The challenge
COVID-19 has emphasised and exacerbated existing health inequalities, and no single issue defines the pandemic more. The pandemic has had an unequal and profound impact on people and communities across the UK.
There is a clear relationship between mortality due to COVID-19 and deprivation, with more deprived areas experiencing higher mortality. A study by Professor Michael Marmot has found that COVID-19 death rates are a quarter higher in Greater Manchester than in the rest of England. 1 His report concludes that the more impoverished a local authority, the higher its mortality rate.
In England, the age-standardised mortality rate for deaths involving COVID-19 in the most deprived areas in July 2020 was 3.1 deaths per 100,000 population. This was more than double the mortality rate in the least deprived areas (1.4 deaths per 100,000 population). 2 This has been described as a ‘gradient of disadvantage,’ with COVID-19 ‘imposed on pre-existing health inequalities’. 3
People with black and minority ethnic (BME) backgrounds have been disproportionately affected by COVID-19. For example, an Intensive Care National Audit and Research Centre (ICNARC) COVID-19 case audit in April 2020 found around 34 per cent of 4,873 critically ill patients were from a BME background, contrasting with 11.6 per cent of patients with viral pneumonia between 2017-19. 4
What have NHS leaders told us?
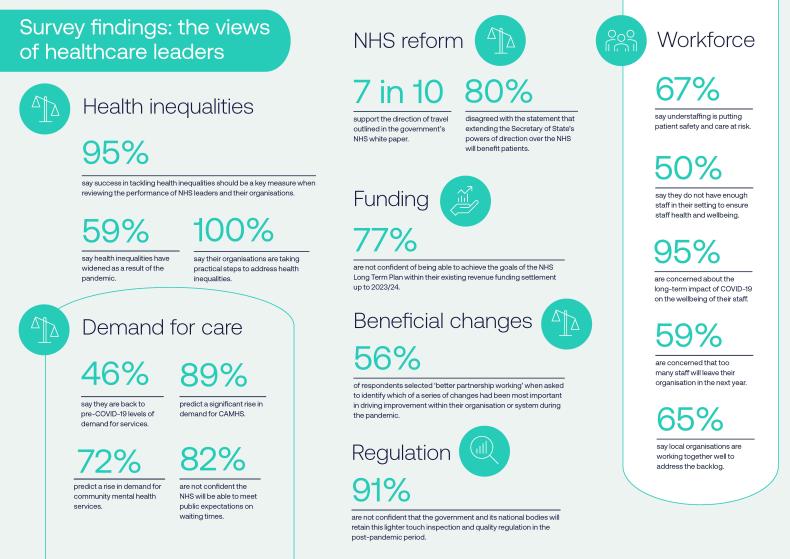
NHS leaders recognise the impact of the pandemic on inequity, with a majority (59 per cent) of our leaders panel saying that health inequalities have increased significantly in their area. NHS leaders know the service must play its role in addressing systemic inequality, unfairness and injustice.
All members of our leaders panel said that the organisation they work for is taking practical steps to address health inequalities, either to some extent or to a great extent. But the complexity of the task relating to health inequalities is not lost on them. One respondent to our survey said it will require a ‘generational change’ in our approach and that it is ‘not like hitting a target.’
Addressing health inequalities will require a 'generational change' in our approach
NHS leaders want to make sure that inequalities are not exacerbated as they address the backlog of care (this is explored in more detail in the next section). Many report that they are starting to embed population health management approaches and working in close partnership with providers of other public services, such as local government, housing and education. This will be an essential requirement to begin to close the gap between the best and worst off.
As part of this, they are analysing data by deprivation, ethnicity and presence of learning disabilities, and boosting access to mental health support. Many NHS leaders outlined how they are targeting COVID-19 vaccination programmes at particular groups, working with faith communities and using communications and engagement approaches to target vaccination messaging at those experiencing the greatest inequalities.
Many local systems are giving careful consideration to their roles and responsibilities around addressing wider determinants of health, with one respondent saying:
“We employ a health inclusion champion GP who works across the system to maximise focus on vulnerable, disadvantaged groups.”
Another explained:
“As an anchor institution we want to develop the skills base in our local communities and draw more local people into our workforce and support as many as possible of the 65 per cent of people with a serious mental illness who want to work into good quality jobs.”
However, when it comes to addressing racial inequalities in health more specifically, half of respondents said they were not confident (50 per cent) that the NHS is now taking the necessary steps to ensure that a focus on tackling racial inequalities in health is among the NHS’s highest priorities.
While progress is being made and this is now much higher up the agenda, it is clear that there is more to do to address this challenge and it will need to be a defining part of the NHS’s long-term response to the pandemic.
What do NHS leaders need?
- Areas of support: Asked what help local systems need to help reduce health inequalities, most respondents pointed to better alignment of incentives (24 per cent), more funding (21 per cent) and more system working (20 per cent). Only 9 per cent thought more guidance and support would help.
- Measuring what matters: There was clear support for using success in tackling health inequalities as a key measure when reviewing the performance of NHS leaders and their organisations, with over nine in ten (95 per cent) either agreeing or strongly agreeing with this proposition.
- Duty to cooperate on heath inequalities: The government should develop a duty to cooperate on improving health inequalities. This would enshrine the goal of tackling health inequalities into law and offer a shared goal that is universally supported across health and care organisations. However, closing equity gaps is a long-term project involving multiple sectors and does not lend itself to easy measurement, so ministers should avoid using blunt metrics here.
- Action is also required to ensure effective community engagement with black and minority ethnic (BME) communities to develop culturally competent services so that sustained and trusted relationships can exist between services and communities.
More generally, a substantial proportion of the causes of health inequalities are outside the direct control of the NHS, which highlights the importance of a cross-sectoral approach. Integrated care systems will play a key role in this agenda and they will need to strengthen the NHS’s links with services outside health and care to achieve the goal of tackling long-standing inequalities in health.
The NHS Confederation will play its part in supporting the NHS to address inequalities. The NHS Race and Health Observatory, which is hosted by the NHS Confederation, has been established to identify and tackle the specific health challenges facing people from BME backgrounds.
Figure 1: What areas do you, your organisation and/or local system need to help reduce health inequalities?
Chapter footnotes
- 1. Marmot, M et al (2021), Building Back Fairer in Greater Manchester: Health Equity and Dignified Lives. London: Institute of Health Equity. https://www.instituteofhealthequity.org/resources-reports/build-back-fairer-in-greater-manchester-health-equity-and-dignified-lives ↑
- 2. Office for National Statistics (2020) Deaths involving COVID-19 by local area and socioeconomic deprivation: deaths occurring between 1 March and 31 July 2020, available online at: https://bit.ly/3ADa48i ↑
- 3. Marmot M, Allen J. COVID-19: exposing and amplifying inequalities J Epidemiol Community Health 2020;74:681-682 ↑
- 4. Intensive Care National Audit and Research Centre (17 April 2020), ICNARC Report on COVID-19 in Critical Care, accessed April 2020 ↑
Recovering the backlog and managing expectations
The challenge
The sustained impact of the pandemic will leave a backlog of care in excess of anything seen over the last decade. Requirements to separate patients on site with COVID-19 from those who are not infected, and other infection prevention and control measures, along with the need to manage staff illness, have meant that providers across all sectors have faced restrictions on their capacity during the pandemic. Depending on how long COVID-19 infection control requirements endure, providers may have to run at lower rates of occupancy than normal for some months to come.
An inevitable consequence is that waiting lists have increased. The waiting list already stood at more than 4 million before the pandemic. It has increased to over 5.6 million people who were waiting to start NHS treatment at the end of July 2021, of whom over 290,000 had been waiting for more than a year. 5
And there are concerns that a large ‘hidden’ waiting list for treatment is not being captured in the data, with over 7 million fewer referrals for elective care having been made during the pandemic than would normally be expected. Many of these will be for conditions that deteriorate over time and have a significant day-to-day impact on patients’ ability to go about normal life. It is important to note that even though the waiting list has increased by 1 million this year, that is not because the missing waiting list has begun to return. It is the result of the elective deficit whereby day-to-day demand is outstripping the NHS’s ability to provide care.
Inequalities are now becoming evident in the backlog, with evidence suggesting that waiting lists have grown more rapidly in more deprived areas during the pandemic. These areas could face disproportionately large waiting lists per head of population, and deprived communities could also have larger numbers of ‘missing’ patients. A separate report from the NHS Confederation, published alongside this report, examines this issue in more detail. In summary, we are seeing a mixed picture across the country but generally, where statistically significant relationships exist, we are seeing evidence that suggests:
- increases in admissions for specialties such as trauma and orthopaedics and ENT associated with areas of less deprivation
- increases in waiting list numbers associated with areas of greater deprivation, especially in neurology, general surgery, and dermatology
- overall levels of waiting per head of population associated with areas of greater deprivation.
More generally, pressure is being felt across all parts of the system, and many services are back to pre-COVID-19 levels of demand, with 46 per cent of survey respondents telling us demand for services was already back at pre-pandemic levels. Many NHS leaders report that they are at winter levels of demand. NHS acute, mental health, community, ambulance and primary care services are all seeing more patients with more complex needs.
Greater demand for primary care and community health services is being experienced due to the impact of long COVID and the rehabilitation support required for those patients undergoing treatment. We are also seeing increases in demand for mental health support. Since the lift in many lockdown restrictions, providers anecdotally report that referrals are rising to above pre-COVID-19 levels, with particular pressure on children and young people’s services. They are seeing patients with more significant needs, a higher proportion of patients accessing services for the first time, and PCNs are also anecdotally reporting a 50 per cent increase in demand for mental health support in primary care. Increased demand is also being seen in emergency settings.
In the next phase of the recovery, mental health service providers are expecting demand from people who would have been referred to services had the pandemic not struck; people requiring more support due to a deterioration of their mental health during the pandemic; and new demand driven by people needing support due to the wider impacts of the pandemic, such as self-isolation, financial insecurity and increases in substance abuse and domestic violence. Around 10 million people are predicted to need new or additional mental health support as a direct consequence of the pandemic over the next three to five years. In particular, there are significant increases in demand for mental health support for children and young people across all services. This includes a 113 per cent increase in children and young people accessing urgent support for eating disorders between April and November 2020.
In addition, there are particular concerns that the stark inequalities faced by BME communities in accessing services and recovery rates, will be exacerbated. 6
What have NHS leaders told us?
Recovering the backlog of care in sustainable ways that avoid overloading NHS staff and exacerbating health inequalities, while also managing public expectations about how long the recovery will take, is among the top concerns of healthcare leaders.
The vast majority of our panel said they expected to see significant increases (i.e. more than 20 per cent) or slight increases (5-20 per cent) in the number of people seeking most acute, ambulance, mental health and community services over the next three years. They are also predicting significant rises in demand for primary care services. This will not come as a surprise, but it underlines the rapid increases in demand that are facing services across all parts of the system.
The service areas where the greatest proportion of our leaders panel predicted a significant rise in demand overall were child and adolescent mental health services (CAMHS) (89 per cent) and community mental health services (73 per cent). The acute service area where the greatest number of respondents predicted major increases in demand was elective care (35 per cent). Nearly two thirds of respondents (63 per cent) predicted a significant rise in demand for primary care GP services and almost half predicted a significant rise in social care (45 per cent). In the community sector, the area where most respondents expected to see major increases in demand was crisis response (46 per cent).
Most respondents (65 per cent) were confident that local organisations in their health and care system were working together sufficiently well to address the backlog of treatment that has built up. And most respondents (59 per cent) agreed that elective care recovery was now being planned in a more nuanced way than before, by targeting both clinical need and health inequalities to reduce harm to patients.
However, of those who said they were not confident that local organisations in their health and care system were working together sufficiently well, respondents highlighted the risk that pressures on acute trusts, including surgery and cancer waiting lists, might leave mental health services in a ‘second tier’ for local system priorities. They also mentioned staff shortages and a lack of capital funding as likely barriers. One respondent said:
“We needed transformative change in the system before the pandemic and now we have taken 100 steps backwards. The work of the last 20 years has been significantly compromised within the last year.”
Another warned about the potential impact of a backlog of patients unable to access primary care, whose size is as yet unclear:
“They are working well enough to address the known backlog, [but] the unknown backlog created by delayed or deferred presentation in general practice is more difficult to quantify. Unless improved primary care access is supported, we will not be able to address the true total backlog. Demand and capacity in general practice are not currently matched and there is no spare capacity for those who have deferred presenting.”
In terms of managing public expectations, more than four in five (82 per cent) respondents did not feel confident that the NHS would be able to meet public expectations on treatment and waiting times. Almost three quarters (73 per cent) did not think there was sufficient funding to deliver safe and effective services. Almost four in five (79 per cent) did not feel confident that the NHS would be able to deal with COVID-19 demands, restore services and manage upcoming winter pressures. This amounts to serious concern that the public will become frustrated by the time it will take the health service to catch up, post-pandemic.
Figure 2: To what extent do you agree with the following statements?
What do NHS leaders need?
Recovering the backlog in sustainable ways that avoid overloading NHS staff and exacerbating inequalities is the priority concern. When asked what factors would make the biggest difference to addressing rising demand for services, the most prominent answers from our leaders panel included:
- A more integrated and targeted approach to population health management: NHS leaders say a focus on producing the necessary data on those who make high use of services and a more integrated and targeted approach to population health management is a key factor that would make the biggest difference to addressing rising demand. This needs to be backed up by more integration between health and social care at the level of pooled budgets.
- Building back fairer: There are good reasons to believe that the current approach to elective care, whereby patients are treated in the order they present for care, exacerbates inequalities, worsens health outcomes and perpetuates the inverse care law. If the NHS is to restore services inclusively, radical action is needed. A separate NHS Confederation report published alongside this report identifies a package of measures.
- The ‘hidden’ waiting list: A priority is to understand the 'missing 7 million’ who did not come forward for care during the pandemic as would otherwise have been expected. We know many of them will be from deprived and marginalised groups. That will require the NHS to grow the backlog in the next few months in order to make sure local services identify all patients that need care. The waiting list will therefore probably get worse before it gets better but, ultimately, this approach will help ensure we are addressing the backlog in a fairer way that doesn't worsen health inequalities. This is crucial as we know it will be people from deprived and marginalised groups who will hold back from seeking care, and that failing to identify the true scale of the issue will exacerbate health inequalities in our communities. Balancing the need to grow lists, while at the same time being clear that increased pressure on NHS staff could cause many on the brink of retirement to leave, is a key challenge for the next three years. Other measures include reforming constitutional standards, promoting active waiting, and using tools to scan for early symptoms of life-threatening conditions as part of routine interactions with patients.
- Financial certainty for October onwards: We have long been calling for the government to confirm the funding the NHS will have from October onwards. This finally came on 6 September when £5.4 billion for the NHS in England was announced. This will provide additional investment to help train theatre staff, recruit skilled waiting list management capacity, and invest in local elective call centre staff to help effectively manage patient communications. Investment in these and other staffing disciplines will speed the recovery and ensure that clinicians in primary and secondary NHS organisations are able to focus on delivering care, not fielding calls from understandably anxious patients.
- Extend discharge-to-assess funding: The confirmation of the NHS’s budget for the second half of the year included vital extra funding of just under £500 million for discharge to assess to be extended. With significant extra demand from patients experiencing long COVID, and with many more patients needing rehabilitation as they recover from operations, this funding is vital to ensure patients can be quickly and safely discharged into the community. More generally, the government needs to recognise the impact of COVID-19 over the longer term by creating specialist long COVID services and expanding community and primary-care-based rehabilitation.
- Access to capital funding: Trusts need to access capital funding now to expand their elective capacity safely and to make A&E departments large enough for social distancing. They need to invest in facilities that will make them more efficient and improve patient care, such as community diagnostic hubs and elective treatment centres, and to make their wards COVID-19 secure. All of this will be vital as we prepare for the expected flu surge this winter. But leaders are either not able to access the capital they need or, if they are, it takes too long to receive, with too many bureaucratic hurdles to overcome. This funding holds the key to unlocking elective and other capacity. We await the capital spending settlement in the Comprehensive Spending Review but, in the short term, clear guidance from NHS England and NHS Improvement – backed by HM Treasury and the Department of Health and Social Care – on what trusts and local systems must do to have their capital plans approved will help NHS leaders quickly make the changes that are needed.
- Frontline mental health services need further funding beyond the £500 million that has been made available, focusing on both early intervention and ensuring that specialist support is in place for those people with the highest levels of need. It is unclear at the time of writing this report whether additional funding for mental health is included in the Spending Review announced on 7 September.
- Managing public expectations: The extra funding handed to the NHS and social care is welcome but, given it falls short of what is needed, leaders need the government to manage public expectations about how long it will take to deal with the care backlog. This was characterised by one panel member as requiring ‘a frank conversation with the public about realistic expectations, increased resource into out-of-hospital management of need, and commissioning of proper prevention services.’
Chapter footnotes
- 5. NHS England (2021), NHS referral to treatment (RTT) waiting times data March 2021 https://www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2021/05/Mar21-RTT-SPN-publication-version-1.pdf ↑
- 6. NHS Confederation (2020), Mental health services and COVID-19: preparing for the rising tide, available online at: https://www.nhsconfed.org/publications/mental-health-services-and-covid-19 ↑
Action on staff shortages and sustained support for health and wellbeing
The challenge
Caring for patients and service users during the pandemic has taken an enormous toll on NHS and social care staff. Throughout this time, there has been a significant focus from NHS organisations and national bodies on placing staff experience and wellbeing at the centre of decision-making. With the NHS facing a major backlog of treatment across all settings and an expected surge in demand for mental health services, this must continue. The ongoing demands of COVID-19 and persistent inequalities across the workforce make clear that such a focus must remain a priority, delivered at local level and enabled by national policy, planning and funding decisions.
For health and care staff, the pandemic has been likened to sprinting a marathon, with concerns raised over the impact on health and wellbeing. Employing organisations within the NHS have worked hard to support the wellbeing of their staff during the pandemic, providing listening sessions, risk assessment, support with finance, and measures to help those who are working from home and those still attending a workplace. These are provided alongside national schemes to offer confidential support, specialist bereavement services and online resources, including helplines designed to meet the specific needs of staff from BME backgrounds who have been particularly badly affected by COVID-19. 7
A focus on staff and their health and wellbeing will therefore need to be at the heart of the pandemic recovery. Such an approach will also need to apply equally to the legislative, policy and structural changes that are planned to the NHS in England. These structural and organisational changes are important but they can have a negative impact on staff, and can exacerbate existing inequalities, if they are not implemented well.
These pressures continue to be exacerbated by long-standing staff shortages. In the three-month period ending in June 2021, total full-time equivalent staff vacancies stood at 93,806, according to NHS England and NHS Improvement data. 8
What have NHS leaders told us?
Concerns over staff shortages and on the health and wellbeing of staff are among the most significant issues for NHS leaders.
Two thirds of leaders (67 per cent) said that understaffing across the NHS is putting patient safety and care at risk. Half (50 per cent) of our leaders panel said they do not have enough staff in their setting to ensure staff health and wellbeing. And the vast majority (95 per cent) are concerned about the long-term impact of COVID-19 on the wellbeing of their staff.
While much government focus is on attracting new staff to the NHS, there is widespread concern among our panel that staff will look to leave the NHS on the back of the pandemic and with the unrelenting pressure that they are now facing in recovering the backlog. Nearly six in ten (59 per cent) of our panel said they are concerned that too many staff will leave their organisation in the next year.
Many NHS leaders also identified negative impacts from new ways of working. There were frequent concerns that remote working had ‘left some staff feeling isolated and lonely,’ and that the impact of not being able to do group activities and organisational development interventions face to face had affected organisations’ ability to improve ‘culture and experience.’ Settling in new team members – and particularly non-executive directors – in a largely digital environment was also viewed as a particular challenge.
More positively, there was much optimism about how organisations were now working together to address staff shortages. Eight in ten respondents said they are pooling their resources and collaborating with other organisations either a little or a lot when it comes to deploying staff, with 15 per cent saying they were doing this a lot.
Figure 3: To what extent do you agree with the following statements?
Figure 4: How much are you pooling resources and collaborating with other local organisations when it comes to deploying staff?
What do NHS leaders need?
- NHS leaders will continue to do everything they can to look after and protect their staff, but in this next phase of the recovery, it is clear the NHS will need a realistic and steady approach to resuming services that explicitly recognises the need for health and care staff to recover.
- Sustained local mental health service support should be put in place for the workforce in addition to what has been offered already, with local leaders being given dedicated funding to come up with their own initiatives for their staff.
- To fully address the wellbeing of staff for the long term, the government will need to address long-standing vacancies. A long-term, costed and funded plan to grow NHS workforce numbers will be required. This is essential if we are to give our teams hope that the staffing pressures they have been working with for many years will now be addressed.
Chapter footnotes
- 7. NHS Confederation (2021) Putting People First: Supporting NHS Staff in the Aftermath of COVID-19, available online at: https://www.nhsconfed.org/publications/putting-people-first ↑
- 8. NHS Digital (2021) NHS Vacancy Statistics April 2015-June 2021 tables, available online: https://digital.nhs.uk/data-and-information/publications/statistical/nhs-vacancies-survey/april-2015---june-2021-experimental-statistics ↑
Accelerating moves to integrated care and system working
The challenge
The experience of recent years, and especially during the pandemic, has shown the very real benefits of collaboration within the NHS and also with other public services. There is consensus among our leaders panel that the complex challenges facing the health and care sector over the coming years will require ever-closer collaboration, risk-sharing and local flexibility.
Our panel report that COVID-19 has accelerated transformational change, much of which has been enabled by the structures and ways of working created through partnerships. Examples include significant re-shaping of acute care services at pace into ‘hot and cold’ COVID-19 sites; triage of referrals; use of advice and guidance as an alternative to referral; huge uptake of online and video consultations; shared leadership from health and care leaders; as well as changes to clinical pathways on an unprecedented scale.
The challenge now is to further embed these ways of working.
What have NHS leaders told us?
When asked to identify which of a series of changes had been most important in driving improvement within their organisation or system during the pandemic, better partnership working was the most commonly chosen answer, with 56 per cent of respondents selecting it. The second most popular answer, with 19 per cent of respondents selecting it, was greater use of digital services for clinical purposes, such as patient consultations.
Leaders felt that their organisations were fully engaged in the work of their integrated care system and supported its priorities. Almost three-quarters (70 per cent) strongly agree that this was the case, with 21 per cent ‘slightly agreeing.’ Only one respondent disagreed with this statement. Two-thirds of our leaders panel (67 per cent) said there is a positive relationship between all organisations within their integrated care system.
There is also broad support among our leaders panel for the direction of travel outlined in the health and care bill. There is clear appetite to ensure NHS, local government, private and voluntary, community and social enterprise organisations can operate as equal partners during the next phase of the recovery. In many ways, healthcare leaders see the type of integrated working envisioned in the bill as already happening to positive effect on the ground within integrated care systems, most notably at neighbourhood and place levels. In that sense, the legislation is playing catch up with the environment, rather than seeking to change it significantly.
However, there was some scepticism about whether structural reorganisation could ever deliver the promised improvements. One NHS leader warned:
“It may be the right thing to do, but it’s so disruptive in a time when most are exhausted.”
NHS leaders have clear concerns in one or two key areas of the legislation, most notably when it comes to proposals to extend the Secretary of State for Health and Social Care’s powers of direction over the NHS. Four in five of our leaders panel (80 per cent) disagreed with the statement that extending the Secretary of State’s powers of direction over the NHS will benefit the health service. And 57 per cent disagree that extending the Secretary of State’s powers to intervene over local service reconfiguration will reduce barriers to necessary reconfiguration.
Views were mixed over whether the white paper would enable integrated care systems to exercise appropriate levels of discretion in decisions about the implementation of national priorities, with 40 per cent agreeing with this statement and 36 per cent disagreeing.
What do NHS leaders need?
The findings from our survey, and from the wider engagement we have had with our members since the start of the pandemic, point to four key areas that require government and national body action:
- An acceleration of ‘system by default’: Now is the right time to empower integrated care systems to drive transformative change. The government and NHS England and NHS Improvement must ensure that we do not lose the vital momentum that has been built up in recent months. That means avoiding delays to the passage of the health and care bill and supporting NHS and care leaders to prepare for integrated care systems becoming statutory bodies in April 2022. The timetable is tight and there is much to do to ensure integrated care systems and their partners are ready. NHS leaders and their partners in local government need clarity to ensure that both the government and NHS England and NHS Improvement can work effectively together with integrated care systems and other NHS leaders to make this next stage of the reforms a success.
- System-level planning: An expectation that all phases of the recovery will require plans to be at a system-level, with local systems being held accountable for the effective use of capacity and demand.
- Population health management: An acknowledgement that population health management will be a critical factor in ensuring that local populations’ health and care needs are met, and in linking services across neighbourhood, place and system level.
- Digital integration: An acknowledgement that this must be underpinned by digital integration across all providers in the system, ensuring that patient data is being used to recognise where health inequalities are adversely affecting health outcomes.
- Caution around excessive ministerial control: The NHS is already one of the most centralised health systems in the world and it would be a mistake to centralise it further. New powers that would enable the Secretary of State for Health and Social Care to intervene in issues such as local service reconfigurations should be removed. If they are to remain, then at minimum there needs to be public transparency on the decisions that are made by the Secretary of State and the evidence base upon which they are made. In our view, this must include a requirement for the Secretary of State to have regard to, and publish, the clinical case offered by the integrated care board in relation to any decision.
A lighter, leaner regulatory culture
The challenge
The pandemic has seen lighter-touch regulation and performance management in use across health and care. This has required less paperwork and reporting and allowed providers to spend more time on providing care for patients, which was crucial at a time of unprecedented challenge.
NHS leaders know the importance of governance and regulation, but also note that overly burdensome regulatory activity can stifle innovation and increase the length of time it takes to get work done.
Following recommendations by the NHS Confederation in March 2020 for a suspension to planned inspections during the pandemic, we were pleased to see that this has been beneficial to providers, reducing bureaucracy and allowing trusts to be more responsive and flexible in how they provide patient care. We are also pleased to see the CQC’s proposed new strategy for regulating systems, which recognises the complexity of doing so.
However, NHS leaders are now starting to see regulatory requirements ramping up again, and they are concerned that some of the beneficial changes from the pandemic when it comes to ‘right touch’ regulation risk being lost.
What have NHS leaders told us?
Just under half of the leaders panel (46 per cent) say they are well supported by national bodies, including NHS England and NHS Improvement, to deliver their services. A quarter (25 per cent) disagree. Just over half (53 per cent) say their conversations with NHS England and NHS Improvement on the performance of their organisation/system are supportive, compared with 16 per cent who say they are unhelpful or highly unhelpful.
Despite this, the vast majority (91 per cent) are not confident that the government and its national bodies will retain this lighter touch inspection and quality regulation in the post-pandemic period.
These findings are also relevant to the government’s proposed health reforms. More than two-thirds (70 per cent) say the government’s NHS white paper represents the right direction of travel for the NHS. In particular, there is widespread support for greater partnership working and the creation of integrated care systems on a statutory footing. For instance, one NHS leader said:
“I believe a real focus on integrated care with increased local autonomy and mutual accountability will ensure a focus on resident, patient and community rather than organisation. The emphasis on transformation and triple aim also points us towards continuous improvement.”
What do NHS leaders need?
- Permissive legislation: There is a widespread view across the NHS that the forthcoming legislation should aim to be as permissive as possible. Central to successful system and partnership working is the idea that local leaders best understand their local communities, economies and health needs. One of the most welcome features of the health and care bill is that it recognises the contribution that local leaders will make to addressing the specific needs of their communities. It is especially welcome, therefore, that the bill provides scope for local flexibility. We urge the government and those who regulate and oversee the NHS to ensure that the bill, and in particular the guidance to support its implementation, continues to embrace this principle.
- Letting local leaders lead: In addition, we urge national regulators to move to a new system of assurance and performance monitoring for providers, commissioners and system leaders that is enabling of local leaders. This includes not returning to the pre-COVID-19 model of inspections led by the CQC. Central to successful system and partnership working is the idea that local leaders best understand their local communities, economies and health needs. Therefore, NHS England and NHS Improvement should agree clear goals and targets with primary care, trusts and systems and allow them to get on with designing and delivering care.
A new financial deal for health and social care
The challenge
The NHS went into the pandemic with serious financial challenges, and these have been exacerbated by the impact of the last 18 months.
While an additional £3 billion of funding was announced in Spending Round 2020 to tackle the elective care backlog, extra demand for mental health, and wider pressures, this fell far short of the £10 billion investment in the NHS that was recommended by the Health Foundation, and supported by our members, to deal with the impact of pressures and fall out from COVID-19 on services.
A report published in early September by the NHS Confederation and NHS Providers, based on a survey of England’s hospital, mental health, community and ambulance service trusts, also identifies that in the next financial year (2022/23) the frontline NHS will need around an extra £10 billion of revenue funding. The extra funding requirement comprises:
- between £4 and £5 billion to cover extra costs driven by COVID-19, estimated in the report as £4.6 billion
- between £3.5 and £4.5 billion for each of the next three financial years to recover the care backlogs created by COVID-19 across elective surgery, cancer, mental health and community services
- recognition that, over the last 18 months, trusts have not been able to make the annual 1.1 per cent efficiency savings assumed in the existing NHS five-year budget, given their overwhelming focus on treating COVID-19 patients and that returning to this level of savings will take time.
This investment is in addition to the costs of delivering the government’s key manifesto commitments of building 40 new hospitals and reforming our overstretched social care system, as well as meeting the ongoing central government bill for COVID-19 activities such as Test and Trace and COVID-19 vaccination.
The government delivered its Spending Review settlement for the NHS and social care in England on 7 September. This provided welcome extra funding for the NHS and social care and will help the NHS to make a start on tackling backlogs. However, the £6.5-7 billion of extra funding it will give the NHS in 2022/23 falls short of the £10 billion we believe is needed.
What have NHS leaders told us?
Members of our leaders panel are growing increasingly concerned about their ability to achieve the goals of the NHS Long Term Plan within current funding levels.
Not a single panel member told us they were ‘very confident’ of being able to achieve the goals of the NHS Long Term Plan within their existing revenue funding settlement up to 2023/24. More than three-quarters of panel members (77 per cent) said they were not confident about achieving this goal. Fewer than one in five (18 per cent) said they were confident.
Many NHS leaders are frustrated that they are struggling to access the capital funding they need to invest in facilities that will make them more efficient and improve patient care. And they are growing increasingly concerned that they do not have the financial certainty they need for the second half of the 2021/22 year. The NHS is being expected to plan care and treatment for patients, and recruit staff, without knowing how much they will have to spend to do so beyond September, when much of the extra COVID-19 funding is due to end. The NHS Confederation wrote to the Chancellor in early July to push for this financial certainty.
In addition, NHS leaders continue to be frustrated at the government’s failure to address funding and capacity shortages in social care. They believe this not only means that hundreds of thousands of vulnerable people aren’t receiving the care and support they need, but that this is impacting on the NHS’s ability to deliver services to patients.
Figure 5: How confident are you in being able to achieve the goals of the NHS Long Term Plan with your existing revenue funding settlement up to 2023/24?
What do NHS leaders need?
Many of the factors needed are outlined in section 2 on recovering the backlog. In summary, the government and national bodies need the following:
- Financial certainty for October onwards: We have long been calling for the government to confirm the funding the NHS will have from October onwards. This finally came on 6 September, when £5.4 billion for the NHS in England was announced. This will provide additional investment to help train theatre staff, recruit skilled waiting list management capacity, and invest in local elective call centre staff to help effectively manage patient communications. Investment in these and other staffing disciplines will speed the recovery and ensure that clinicians in primary and secondary NHS organisations are able to focus on delivering care, not fielding calls from understandably anxious patients.
- Access to capital funding: This is crucial so that trusts can expand their elective capacity safely, make A&E departments large enough for social distancing, and expand primary care’s capacity to deal with the rapidly rising demand. We await the capital spending settlement in the Comprehensive Spending Review due at the end of October 2021.
- Deliver a fully funded digital strategy which connects systems and enables the collection of population health data to help move resources to those most in need.
- Revenue funding: More fundamentally, the government’s extra funding announced for the NHS on 7 September is welcome and will help in addressing the backlog. But it falls short of what is needed and it is predicated on COVID-19 infection levels being significantly reduced next year. It is to be hoped that this is the case, but if it is not then the funding settlement will need to be revisited.
Building back better
COVID-19 has shone an unforgiving light on preventable, unfair and avoidable inequalities in health and access to care that had been affecting some people in the UK even before the pandemic began. The pandemic also highlighted areas of strain within the health and care service. The health and care workforce has achieved a vast amount during the pandemic, at significant personal cost with some losing their lives. It is now time for us to repay them by recognising their contribution, giving them time to recover and strengthening the NHS that they have demonstrated so much commitment to.
NHS leaders know that we can no longer permit unjust gaps in health status between the best off and worst off in our country
The findings in this report have identified six areas where we believe that action taken now has the potential to set the NHS and wider health and care system on a more sustainable footing as we begin the post-COVID-19 recovery. Most significantly, NHS leaders know that we can no longer permit unjust gaps in health status between the best off and worst off in our country. We must embrace a population health management approach to ensure that inequities, whether relating to deprivation, race, gender, geography or any other aspect of people’s lives, are addressed. NHS leaders are prepared to be accountable for this objective, provided this accountability is meaningful and realistic, given the complexity and challenge of the task.
As part of this, there needs to be a different approach to tackling the elective care backlog. There are good reasons to believe that the current approach, whereby patients are treated in the order they present for care, exacerbates inequalities, worsens health outcomes and perpetuates the inverse care law. If the NHS is to restore services inclusively, radical action is now needed.
A separate NHS Confederation report published alongside this report identifies a package of measures. A priority is to find the missing 7 million who did not come forward for care during the pandemic as would otherwise have been expected. We know many of them will be from deprived and marginalised groups. That will require the NHS to grow the backlog in the next few months in order to make sure local services identify all patients that need care.
The NHS is based on the founding principles of care being free at the point of use, on the basis of need and not ability to pay. For the NHS to live up to its founding principles, we need a new approach to dealing with the backlog that is based on targeting those in most need, and not solely responding to demand for care from those who come forward. NHS leaders and their teams will play their part, but they need the government and its national bodies to address long-standing staff vacancies, gaps in capital funding, accelerate moves to integrated care and system working, and to create an environment in which local leaders are empowered to lead.
NHS leaders require political leaders to level with the public about the scale of the recovery challenge
The government has responded to our calls for additional investment in the NHS and social care. They have provided welcome extra funding, but it falls short of what is needed. And the extra funding levels are predicated on COVID-19 infection levels being significantly reduced next year, which we can only hope will be the case.
There will now inevitably be difficult decisions between the demands of elective recovery, mental health and the generational task of reducing health inequalities. That is why NHS leaders require political leaders to level with the public about the scale of the recovery challenge. If the government is going to be true to its word of building back better, then it needs to be honest and up front with the public that this will take years to achieve.
There is much good practice emerging from the pandemic to build on. And, crucially, we have a rare policy consensus on the direction of travel, with NHS leaders broadly supporting the legislative reforms that will bolster moves to integrate care. We must not waste this opportunity.
What healthcare leaders need: ten-point plan

Population health: We need to adopt a more integrated, place-based and preventative approach to population health and wellbeing. This will require a population health management approach backed by investment for those areas with greatest need. The establishment of a cross-governmental ministerial board on prevention needs to develop a government-wide strategy on health inequalities, which in turn should work alongside national and local system leadership and accountability with a focus on the wider social determinants of health, to narrow the gap in health outcomes for more deprived communities.

Recovering the backlog: There are more than 7 million fewer patients coming forward for care because of the pandemic. We need to find the 'missing 7 million’ as we know many of them will most likely be from deprived and marginalised groups. That will require the NHS to grow the backlog in the next few months in order to make sure we identify all patients that need care. The waiting list will get worse before it gets better but, ultimately, this approach will help ensure we are addressing the backlog in a fairer way that does not worsen health inequalities. To support these efforts, the government should develop a duty to cooperate on improving health inequalities. This would enshrine the goal of tackling health inequalities into law and offer a shared goal that is universally supported across health and care organisations.

Whole-system solutions: The pressures felt across all parts of the system can only be overcome by working in a truly integrated way. Despite the pressures, NHS leaders and their teams are delivering innovative changes to patient pathways to improve both quality and responsiveness. Examples include new intermediate pathways for children and young people presenting with an eating disorder to avoid admission; effective use of nurse triage models in rapid assessment areas; same-day access to diagnostics; better use of advice and guidance with generalists and specialists working better together to avoid admission; and effective management of the patient treatment list by sharing patient data.

Financial certainty for the long term: Our report with NHS Providers estimates that the NHS will need £10 billion next year as a result of higher day-to-day running costs driven by COVID-19; the extra costs required to clear the backlog of care; and from planned-for efficiency savings not being achievable due to the ongoing demands of COVID-19. This is on top of other key areas of investment that are required in capital, training and education, and social care reform. The government’s Spending Review has delivered some of this funding but not all of it, and a funding shortfall remains. There is also missing clarity on capital spending which is not included in this settlement.

Long-term workforce plan: A long-term, costed and funded plan to grow NHS workforce numbers is required. This is essential if we are to give our teams hope that the staffing pressures they have been working with for many years will now be addressed. This needs to be backed up by sustained local mental health support for staff in addition to what has been offered already, with local leaders being given dedicated funding to come up with their own initiatives for their staff. The duty outlined in the draft health and care bill for the Secretary of State for Health and Social Care to publish, at least once every five years, a report describing the system in place for assessing and meeting the workforce needs of the NHS, is insufficient and far too infrequent.

Addressing the mental health pandemic: With 10 million people predicted to need new or additional mental health support as a direct consequence of the pandemic over the next three to five years, frontline mental health services need further funding while also focusing on early intervention and ensuring that specialist support is in place for those service users with the highest levels of need.

Accelerate system by default: Now is the time to empower integrated care systems to drive transformative change. That means avoiding delays to the health and social care bill and supporting leaders to prepare for integrated care systems becoming statutory bodies in April 2022. The timetable is tight and there is much to do to ensure integrated care systems and their partners are ready. There is, however, only so much that can be drafted in legislation, so carefully crafted guidance and support will be needed.

Maintaining 'right touch' regulation: Political and national leaders need to create a lighter, leaner, regulatory culture that empowers local leaders to lead, and which reduces unnecessary interference from the government and its national bodies. This means the government must avoid returning the NHS to an environment in which there is excessive ministerial involvement. Instead, NHS England and NHS Improvement and other regulators should agree clear goals and outcome-focused targets with NHS organisations and allow them to get on with delivering care. As part of this, the national bodies should build on recent attempts to create a no-blame culture in the NHS that enables leaders and their staff to raise concerns and seek help from their peers and national experts, without fear of reprisal.

Digital integration: All of this must be underpinned by digital integration across providers in systems, ensuring that patient data is being used to recognise where health inequalities are adversely affecting health outcomes.

Managing public expectations: There will have to be difficult decisions between the demands of elective recovery, access to primary care, mental health and the generational task of reducing health inequalities. That is why NHS leaders require the government to level with the public about the scale of the recovery challenge. If the government is going to be true to its word of ‘building back better,’ it needs to be honest and up front with the public that this will take years to achieve. Clearing the elective backlog alone will take five-to-seven, not two-to-three, years. We also need honesty that the NHS cannot improve the nation’s health on its own. We need transport, economic, education and food policy to align across government and to contribute to the wider ambition of healthier families living happier lives.
About us
We are the membership organisation that brings together, supports and speaks for the whole healthcare system in England, Wales and Northern Ireland. The members we represent employ 1.5 million staff, care for more than 1 million patients a day and control £150 billion of public expenditure. We promote collaboration and partnership working as the key to improving population health, delivering high-quality care and reducing health inequalities. Find out more about what we do.
NHS Reset is our campaign to help shape what the health and care system should look like in the aftermath of the pandemic. Recognising the sacrifices and achievements of the COVID-19 period, it brings together NHS Confederation members and partners to look at how we rebuild local systems and reset the way we plan, commission and deliver health and care. Find out more about the campaign.