Key points
Much has changed in the 75 years since the NHS was founded – from shifts in NHS staffing, lifespans and disease burden, to public expectations and technological innovation. With the health and care sector at a crossroads, the time has come for an ambitious new social contract that empowers the public to take greater control of their own health and experience of care.
Technology holds promise for the future of healthcare. It can prevent illness, enable early diagnosis, empower health management and support general wellbeing. But how might people use technology to have more control over their health and wellbeing? And do they want to?
To uncover the answers to these questions, the NHS Confederation, in partnership with Google Health, commissioned Ipsos to explore people’s behaviours, attitudes and beliefs about responsibility and control when it comes to their health, the role that health technologies play in this, along with their expectations about the future of healthcare.
A survey of more than 1,000 adults in the UK – a third of whom live with one or more long-term conditions (LTCs) – and interviews with individuals with LTCs and who have frequent interaction with the health system, form the centrepiece of this report.
While individuals feel accountable for their health and wellbeing and want to be empowered to improve it, what became evident is that, frequently, they lack the confidence, tools and technologies to take control as much as they would like.
We heard that people want more control over their health but need their actions, and the tools they can use, to be endorsed by healthcare professionals. They also want to make better use of health technology, but not at the expense of face-to-face contact with their doctor or other healthcare worker.
While the vast majority of people use some form of health technology and find that useful, they are not totally satisfied by what is currently on offer.
Across all age groups more than 7 out of 10 (72 per cent) would use technology to avoid a hospital admission, with a similar proportion happy to use technology to monitor their health and share information and data with their doctors.
Many individuals are not confident about using technology to manage their health, leading to a fear that they may be locked out of healthcare if they cannot access or use digital tools.
People think there is a larger role for health technologies in the future; many are not confident in using them now.
Three areas emerged as necessary building blocks that could enable greater patient empowerment: digital access and inclusion, patient satisfaction, and user confidence.
This first report concludes that the health service must design services in collaboration with patients to address these issues and empower patients. The next phase will explore health leaders’ and practitioners’ experiences and views and identify practical examples that speak to resetting the social contract between the public and the NHS.

Forewords
Introduction
As the NHS marks its 75th anniversary, it faces unprecedented challenges. Even before the COVID-19 pandemic, the health and care system was under significant pressure. NHS staff vacancies stood at 90,000, with a further 120,000 in social care. Both have since risen. Waiting lists have grown to a record high of 7.3 million, up from 4.6 million in February 2020. And year-on-year demand has followed an upward trend. These changes, both in demand for services and capacity to deliver them, have increased pressure on the system, with public satisfaction at a 25-year low.
When the NHS was founded in 1948, the prevailing model was one of delivering episodic care, largely provided through patients being admitted to hospital or visiting their GP. This approach has remained largely intact to the present day. However, a combination of shifts – in NHS staffing, in lifespans and the disease burden, in public expectations and technological innovation – means the NHS needs to shift to a new service model, fit for the 21st century.
The question of accountability is central not just to alleviating these pressures but to meeting population health needs and expectations, as the NHS Confederation’s Matthew Taylor recently explained:
"While there is an inevitable hierarchy in the NHS as a publicly funded, politically overseen system… the current model of accountability remains overwhelmingly about what each level owes upwards to the layer above. Instead, we need to see accountability as something we owe outward and downward, just as much as upwards… ultimately [this] means a service that is orientated to empowering and enabling patients and communities to improve their health and wellbeing.”
In empowering patients and forging a new social contract with the public, expanding the use and range of digital alternatives alongside face-to-face care – including telecare, virtual wards, remote monitoring, wearables and hands-free tech, among others – presents a range of opportunities. These technologies can help to support citizens and communities in prevention, early diagnosis, long-term condition management and general wellbeing.
Context
The NHS Long Term Plan set out the NHS’s aspirations for a digitally transformed and sustainable health and social care system. This included taking a leap forward in its digital ambitions, transforming the way care is delivered by organisations and experienced by patients and populations. Supported by the merger of NHSX and NHS Digital into NHS England, integrated care systems (ICSs) have been charged with planning and delivering joined-up health and care services in their area, including developing a system-wide local digital strategy. Meanwhile, national policies, through the What Good Looks Like framework, have provided ICSs with guidance on co-designing digital-first approaches with their local population.
Despite some good progress, in early 2023 the House of Commons Health and Social Care Committee’s evaluation of government commitments on NHS digitisation concluded that this progress has not been made in all areas. It warned that delegating responsibility for local digitisation without clear expectations or sufficient resources risks increasing variability in digital capacity and capability. Tackling this will be critical if ICSs are to fulfil their potential to both empower local communities, reduce health inequalities and drive digital transformation.
The building blocks for patient empowerment
Over the past decade, the NHS has taken deliberate steps towards a new model of care that focuses on prevention and managing care in the community. This shift has increasingly placed patients at the centre of their own care, enabled and empowered by technology. This approach has had some success to date and many examples of good practice exist, but further and faster progress is needed to embed this service model across the entire system. This will require greater focus on individuals’ ambitions and needs as well as creating sustainable services.
That’s why the NHS Confederation has partnered with Google Health to explore the role of technology in patient empowerment. We commissioned Ipsos to undertake research to understand people’s attitudes to responsibility and control over their health; to uncover their expectations, wants and needs from the health system and technology; and to understand their hopes for the future. By putting people at the centre, our hope is that the insights support the co-design of solutions that meet people’s needs and ensure the sustainability of the health service.
What this work highlights is that the public wants to embrace technology – as they have done in many other areas of their lives – allowing them to take greater control of their health and wellbeing.
The research has identified three main building blocks that any redesign will need to incorporate and build on if the shift to patient-centred care is to be successful:
- ensuring digital access and inclusion
- driving patient satisfaction; and,
- increasing user confidence.
The insights from the research that make up these building blocks, along with the potential implications, are explored in detail later in the report
Research methodology
We commissioned Ipsos to undertake quantitative and qualitative research to:
- uncover the public’s understanding, attitudes and beliefs about responsibility and control over their health
- explore the impact of health technologies and citizen expectations, needs and ambitions
- understand attitudes and future needs with respect to health data and privacy.
Ipsos conducted an online survey among 1,037 adults (18+) in the UK (see figures 1 and 2 for the breakdown by age and gender). Around a third, 332 of these respondents, have been diagnosed with a long- term condition; of those, 92 respondents had a long-term health condition resulting in them interacting with the health system four or more times a year. In addition to the online survey, qualitative interviews were conducted with seven respondents with long-term health conditions and frequent interaction with the health system. All fieldwork took place between March and April 2023.
The quantitative research provides clear insights into how both the general public and, more specifically, those with long-term health conditions think about managing their health today. The data encompass the sense of responsibility they feel for their wellbeing, how this aligns with their feelings of control over their health, and how they hope to see healthcare delivered in the future. Selected findings from the research are included in this report; where appropriate these are presented using a Top 2 Box (T2B) score.*
The qualitative interviews provide clarity on the experiences of those people living with long-term conditions, drawing on lived examples of the distinct ways in which they interact with the health system, use technology to support their health and wellbeing, and their viewpoint on the future of the NHS. Patients came from a range of ages, ethnicities and socio-economic backgrounds. Each has a long-term condition and interacts with the health system regularly. All use technology related to their health condition.
A detailed breakdown of survey and interview findings can be found in our data pack.
* The Top2Box (T2b) is an industry standard where the top two results (for example, strongly agree and slightly agree) of a five-point scale are combined.
Survey findings at a glance
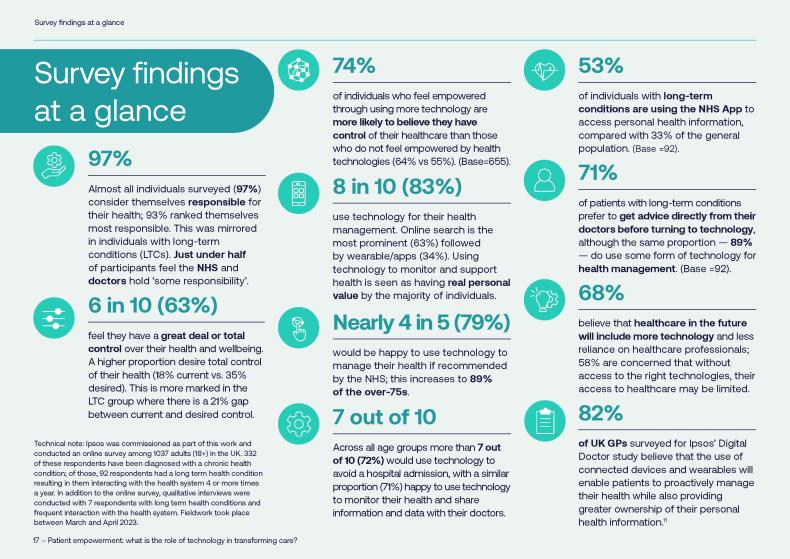
*Technical note: Digital Doctor: Running since 2015, Digital Doctor is a multi-country study among primary care physicians, paediatricians, oncologists, and
neurologists focusing on perceptions and views of digital and connected health. Ipsos conducted a new wave between October 2022 and March 2023 in the form of an online survey among 3428 healthcare professionals across 20 markets. In the UK, the sample was made of: 100 PCPs, 70 paediatricians, 61 oncologists, 60 neurologists. For respondents to qualify, they had to have 2-35 years’ experience in their current role, be over 25 years old and paediatricians had to recommend/ prescribe/administer vaccines.
Ensuring digital access and inclusion
There are disparities in how digital technologies are accessed and used in health, relating largely to age and socio-economic status. Adopting a digital-first approach therefore risks excluding groups of individuals from the care they need.
All technology solutions focused on empowering people to take more control of their healthcare will need to have digital access and inclusion front and centre of the design.
What we discovered
63 per cent of adults over 55 years see healthcare professionals as their first port of call when it comes to managing their health, with more than a quarter (29 per cent) of 66–75 year olds typically using no technology in the day-to-day management of their health, rising to more than one third (35 per cent) of the over 75 year age group. With this reliance on face-to-face contact and lack of technology use, we can see that older adults are at significant risk of digital exclusion.
The lack of usage by older adults is seen across a wide range of technologies – from online searches and seeking health information podcasts through to the use of wearables – with their younger counterparts being far more likely to use these different technologies.
Older people rely heavily on friends and family – including the younger generation – for support around technology. We heard from one of our focus group participants of their reliance on their grandson for help:
“My wife and children and grandchildren encourage my technology use – my 11-year-old grandson is better at it than me.” Male, 75 years old, hypertension, type 2 diabetes, depression
Older adults remain more inclined to seek the advice of a healthcare professional before considering the use of technology, whereas younger adults typically exhaust online information before accessing help from a healthcare professional (61 per cent of 18–35 year olds vs 34 per cent of the over-75s).
What might this mean?
While our research has provided helpful insights, it is limited in what it has told us about some of the main consumers of health services, such as those with dementia, people experiencing homelessness or addiction issues, people with learning difficulties and those who would need the questions translating into another language among others. We also know that these groups, along with older adults, frequently live with long-term conditions and are among those who need the most access to health and care services. Given this, any proposals that come from this work will need to be broadened to include the views and needs of these individuals.
Opportunities to build approaches to increase digital access did start to emerge from the research. We found that older adults really take note of what their doctors say: encouraging them to use health technologies; and 9 out of 10 (89 per cent) would be willing to try technology if recommended by the NHS. It is clear, therefore, that any pathway redesign that includes older patients cannot just be digital; the personal connection with a healthcare professional remains critical.
There will need to be further exploration of the reasons different groups are not currently using technology to support their health – for instance, a greater reliance on other sources of information such as healthcare professionals, friends or family, or the lack of a smartphone, or a lack of trust or confidence in the technology.
Delivering patient satisfaction
The majority of individuals – especially those with long-term conditions – use some form of health technology currently and would be happy to use more, particularly if this enabled them to self-care and avoid hospital admissions. Ensuring individuals have tools that are fit-for-purpose and fulfil their needs is clearly important; there is significant scope to increase satisfaction and drive sustained usage.
What we discovered
8 out of 10 (83 per cent) adults use some form of technology to manage their health, increasing to 9 out of 10 (89 per cent) of individuals with one or more long-term condition. Despite this level of usage, only half (52 per cent) are satisfied with the technologies and tools currently available for them to use; however, it is clear from our focus groups that when the right technology is provided, it can be hugely helpful:
“Technology empowers you! When you have the right kind of technology it helps a lot and makes you feel like you’re taking control!”. Female, 46–55 years old, hypertension
The highest levels of satisfaction with what is currently available are seen in the employed population (56 per cent) dipping down to 41 per cent in the unemployed, 32 per cent in home-makers and 43 per cent in the student population. This may reflect the cost of technologies that are not currently available via the NHS; there is a risk that these high levels of dissatisfaction exacerbate the likelihood of digital exclusion in these groups who potentially have greater needs.
Nearly three-quarters (73 per cent) of patients want their doctors to provide them with the “best technology available”, with three-fifths (58 per cent) wishing “their doctor provided them with technology to monitor their health”. Ease of appointment booking and the ability to communicate via messaging services with healthcare teams are also high on the wishlists of individuals surveyed.
The individuals who took part in the focus group discussions, all of whom are managing long-term conditions and some of whom are very proactive in doing so, are acutely aware of how dependent they are on access to appointments, tests and accurate information. Most raised issues around waiting times and difficulties seeing the same GP. A smoother and more straightforward approach to booking appointments – both in primary and secondary care – along with simple prompts like appointment and prescription refill reminders were all cited as things that would improve the ability of individuals to better lead fuller lives without their long-term conditions dominating.
What might this mean?
Over two-thirds (69 per cent) of people would like to be able to access reliable health information online or via an app; and approximately the same number (66 per cent) want one tool to bring all health information together in one place. The NHS App and NHS website clearly have a role to play here. The NHS App is one of the most downloaded health apps, in large part due to the COVID-19 pass. With a redesign of the app underway to improve user experience, there is an opportunity to meet these ambitions. The recent move to ensuring personal health information is available on the app, along with the new appointment booking feature announced in May 2023, are tapping into the user needs we heard.
It will be important to explore in more detail the lower rates of satisfaction among respondents who were unemployed and to what degree this may or may not relate to their ability to access good technology or technology at all. We know from the quantitative research that there was a desire for GPs to be able to provide better technology to people to enable them to take control of their health and wellbeing.
Comments made in the qualitative interviews reflect that there would be a greater willingness to use technology, such as blood pressure monitors, were they provided by their local surgery. This warrants further exploration, as well as how technology can be improved to support ease of use, and what ways technology can practically and realistically be made available to patients.
Building user confidence
There is widespread acceptance of the need to use health technologies. To increase the actual usage of digital tools, there is a need to ensure confidence in how individuals’ personal health information is used. Many individuals also lack confidence in how to use technology. There is an opportunity for trusted healthcare professionals to guide and train patients to use digital tools effectively.
What we discovered
With the increased use of technology, there is a need to provide individuals with confidence around how their personal health data is used and shared. 59 per cent of individuals expressed
concern about their health information remaining private – a figure consistent across all ages – while accepting that collection of personal health information is inevitable. Just over half of people (47 per cent) say they don’t mind their data being collected if they can see a personal benefit, but this leaves just under half who do not agree with this sentiment. This underlines the need for continued assurance around data use and the safeguards that are in place to protect patient confidentiality.
“As long as it benefits me and doesn’t feel intrusive, then it’s fine [to share personal data].” Male, 24–35 years old, type 2 diabetes, chronic back pain, depression
“As long as my personal data is secure and isn’t just being handed out to anyone, then it’s ok. I always read all the T&Cs on apps.” Male, 55–69 years old, type 2 diabetes
“I don’t like having my information out there, I want to keep it to the bare minimum.” Female, 46–55 years old, hypertension
As well as wanting to know that personal data is secure, individuals also want reassurance and guidance on how to use digital tools and technology properly. Having the right technology is empowering for the majority of individuals; however, there is a marked variation relating to age, with only 48 per cent of over-55 year-olds feeling that way compared with 68 per cent of the 18– 25–year old age grouping.
Having ready access to different technologies in the future – from wearables to reliable online information – increases the confidence of individuals to better self-manage their health. This is much more pronounced in younger age groups, with smaller increases in confidence predicted by older age groups. Combined with the lack of technology usage discussed earlier by older adults, this could clearly contribute to the risk of digital exclusion discussed earlier.
The intervention of a doctor has the greatest impact on persuading individuals to test and adopt technologies – 55 per cent compared with the influence of friends at only 14 per cent. This influence is most pronounced in the over-75 age group at 81 per cent. This level of influence is clearly linked to the personal connection with the individual’s healthcare professional, with less than 25 per cent of individuals being influenced by the broader category of ‘the NHS’.
As well as healthcare professionals having a role in increasing patients’ confidence levels, developers of health technologies also have significant responsibilities in developing intuitive and easy-to- use interfaces, ensuring easy integration for healthcare professionals and in assuring data protection.
There is also a need to work with doctors to increase their confidence in how their patients use technology. In a separate study by Ipsos, the Ipsos Digital Doctor Study 2023, the top concern expressed by the GPs surveyed, at 49 per cent, was that patients may misinterpret data [ 1 ], with the second ranked, at 28 per cent, that there will be excess patient generated data. Doctors, other healthcare professionals and patients are going to have to work in partnership to alleviate the fears on all sides.
What might this mean?
We saw that 63 per cent of individuals use online searches to find out health information, with younger adults in particular exhausting this as a route before seeking health interventions (61 per cent).
Having access to authoritative, high-calibre information is extremely important; we know that information is a determinant of health. The publication, in 2022, of two documents – the position paper from the Academy of Medical Royal Colleges on the principles and attributes of ensuring the credibility of health information on social media, along with the NHS Standard for creating health content – has helped to start driving up the quality of both written and video content.
It will be important to explore all the ways in which individuals’ confidence can be enhanced to enable them to make the most of the opportunities technology can provide. This may, in part, be support the NHS can provide.
Chapter footnotes
- 1. ii. Q9a. Of the concerns you have selected around the use of connected health devices and tools, please select your top three that cause you the most concern. Base: W3’23: All respondents (n=78) ↑
Making progress
Understanding the operating context
Delivering healthcare has always been complex; this has never been more true than now, given the challenges health and care leaders face in the aftermath of the COVID-19 pandemic. At the NHS Confederation, we represent the whole health system and are able to facilitate the cross-system conversations that are needed to decide where resources should be focused.
We know digital transformation and the right use of technology are at the heart of the solution to improve outcomes for patients and deliver a sustainable health service. The recent review of integrated care systems by former health secretary and integrated care board (ICB) chair Patricia Hewitt, talks about the role of data and digital tools to support the prevention of ill health, including establishing minimum data-sharing standards. We are now working with our system leaders and NHS England to support them in how they can implement these recommendations and make a real difference to patients and the services they receive.
The NHS Confederation has a strong focus on digital, data and innovation, and we have been working with our members following the government’s publication of A Plan for Digital Health and Social Care 2022, bringing together digital transformation ambitions for both health and social care. This includes our report last year on what our members need to deliver system-wide digital ambitions, and our recent report exploring the critical success factors for realising the ambitions of the virtual wards programme.
Last year we also launched our Digital ICS support programme in partnership with NHS Providers and Public Digital, with the support of Health Education England, as well as running our ICB digital leaders forum to share best practice and provide a cohesive view on system-wide digital challenges and opportunities. We have worked with our mental health members on digital inclusion to increase choice and improve access to digital mental health services. We have set up a data and digital design group for our primary care members to share and promote the use of digital technology in the delivery of patient care. We have shared best practice and case studies, supporting members as they seek to adopt and maximise the opportunities to improve patient care through collaboration, innovation and technology.
Issues for the health system
If we are to empower people to gain control over their own health and wellbeing as this research has identified many want, we will need to engage broadly with communities and patient groups to co-design future solutions.
Nearly three-quarters (73 per cent) of survey respondents wish their doctors had the best technology to better support them. We need to explore what this means in terms of the technical expertise needed within the healthcare profession. It is clear that for many people this is not a case of either/or – technology or engaging with health-care professionals – but the right combination of both.
How much could and should healthcare professionals be expected to show patients how to use certain technologies? What does this mean for digital skills training across the health and care sector?
And more fundamentally, how does the NHS think about budgeting for a digitally-enabled care model, when many of the benefits are potentially years down the line? These are just a small example of the challenges the government, NHS England and our members will have to wrestle with.
Next steps
In the next phase of this work, the NHS Confederation, supported by Google Health, will work with healthcare leaders, practitioners and patients to explore their experiences and views of how we turn these insights into real change. At the heart of this work will be the search for practical ideas and examples that speak to resetting the social contract between the public and the NHS.
We will engage with a wide group of our health and care leader members to seek their views on their experiences to date of working with patients using technology to access healthcare, manage health conditions and keep well. We will explore what this additional research might mean for their patients as well as the services they currently provide; and understand what healthcare professionals will need in the future, as well as what patients will require. The majority of our members are already on a digital transformation journey; we will continue to support them to help create sustainable services that use digital technology to give patients the control over their that they desire and which provides long-term successful outcomes for both the NHS and our society.
About us
NHS Confederation
The NHS Confederation is the membership organisation that brings together, supports and speaks for the whole healthcare system in England, Wales and Northern Ireland. The members we represent employ 1.5 million staff, care for more than 1 million patients a day and control £150 billion of public expenditure. We promote collaboration and partnership working as the key to improving population health, delivering high-quality care and reducing health inequalities.
For more information visit www.nhsconfed.org

Google Health
Google Health is committed to helping everyone, everywhere be healthier through products and services that connect and bring meaning to health information. At Google Health, we’re deploying tools and initiatives that are designed to help everyone make more informed health decisions for themselves and their loved ones.
By making authoritative information more accessible, assisting the broader scientific community, and leveraging Google’s powerful technologies, we can help people live healthier lives.
For more information visit www.health.google

About this report
This report is the first output of a two-stage project being undertaken by the NHS Confederation and Google Health. It aims to better understand public and patient use of technology in relation to their health and broader attitudes and concerns about health management now and in the future.
The NHS Confederation is responsible for the editorial content of this report.


