Key points
Virtual wards are increasingly being used by the NHS to provide care to patients where they live, whether in a care setting or at home. The NHS has been set a target of 40–50 virtual wards per 100,000 people and, more immediately, to scale up capacity ahead of next winter, to above 10,000 beds by this autumn. This report sets out the critical factors needed to enable the NHS to succeed in achieving these targets and to make virtual wards a sustainable model in the longer term, where patient demand and satisfaction are met, as well as better productivity.
It sets out the findings of research involving a range of NHS leaders, including integrated care system (ICS) chairs and chief executives, integrated care board (ICB) digital leads, clinicians, and senior operational and finance staff. It focuses on the delivery process of virtual wards; the opportunities they bring to the quality of care and impact on demand; the challenges leaders face in implementing virtual wards, including the implications for the NHS workforce; and potential solutions to improving virtual wards as they become commonplace in the NHS.
To be truly impactful on both patients’ quality of care and NHS productivity, it must be recognised that there is a severe workforce and skills shortage in the NHS which is impacting on systems’ ability to fully develop, deliver and scale the full ambition of virtual wards. While we await both the national workforce plan and the digital, data and technology workforce plan, it cannot be underestimated how this steady lack of available workforce over the years continues to affect the feasibility of delivering virtual wards at scale.
Virtual ward staffing needs to be properly planned. Long-term establishments should be set and regularly reviewed for virtual wards and staffing plans implemented, which provide both permanent and secondment-based opportunities for clinical staff (including from social, community and primary care). This will help reinforce the role of virtual wards as a permanent service which can offer real benefits to career development. Placements for students should include exposure to virtual wards alongside other traditional placements.
The government and NHS England should approach virtual ward expansion as a coherent larger-scale and holistic digital project. There is considerable enthusiasm among clinicians and local health leaders for increasing the use of virtual wards; their experience shows that when done well, virtual wards can help keep people out of hospital, discharge patients early, reduce clinical time and give patients autonomy and choice.
In implementing new virtual wards, local providers should ensure that clinicians and patients are involved in co-design from the start of development. Successful examples of virtual wards have depended on creating understanding, confidence and credibility among patients and clinicians, and work best when people identified for virtual ward care being supported through admission by their clinician.
For virtual wards to fulfil their potential to relieve pressure on the NHS in winter 2023, local data should be used to make bespoke, local healthcare decisions that address the needs of that population in every ICS. Currently the potential for increasing effective use of virtual wards is undermined by lack of access to good data on local population needs and demands.
NHS England should be less prescriptive about condition specific virtual ward pathways and allow local systems greater flexibility to deliver and monitor virtual ward models which reflect specific population health needs. The overwhelming focus on respiratory infection and frailty pathways undermine systems’ ability for a more flexible approach. This could harness virtual care in other areas of the NHS beyond acute care, including mental health, primary and community care. This less rigid approach would need to be informed by the wider social care gap that impacts on a wider range of patients outside hospital settings.
ICSs leaders should promote the use of ‘virtual ward champions’ to spread awareness across the hospital and multidisciplinary and integrated care pathways. Our participants found that this was an effective way of marshalling the good will and ability of senior clinicians and consultants who have a long-term investment in their success.
Investment in virtual wards need to be long-term and flexible. In addition, adequate social care support is essential in delivering fully integrated successful virtual wards. Currently, short-term funding models are hindering recruitment, planning and impact assessment of virtual wards. The absence of adequate funding for social care funding is preventing systems from fully addressing the holistic and wrap-around needs of patients away from only clinical virtual ward support.

What are virtual wards?
A virtual ward uses the systems and staffing of a hospital ward while enabling the patient to get the care they need where they live (including care homes) safely and conveniently, rather than being in hospital.
The concept was developed in Croydon Primary Care Trust in South London in the early 2000s and is now in place in many parts of England, supporting people with a range of types of care, for example, frailty or acute respiratory infection. The key aims of virtual wards are to:
- act on evidence-based forecasts from predictive risk modelling to reduce non-elective secondary care (acute hospital) usage
- provide multidisciplinary case management
- serve as a communications hub for all those involved in the care for these complex patients
- offer intuitive working systems that appeal to patients and clinicians alike.
Like a hospital ward, the capacity of the ward is set, and patients are admitted and discharged from those beds. The ward is termed ‘virtual’ as these beds are not real, and care takes place in the most appropriate setting for the patient, usually at home. Initially, patients at highest risk of admission to hospital are considered for admission to the ward and for intensive case management. When one of these ‘beds’ becomes vacant as the patient stabilises, the predictive algorithm is looked to for a replacement.
The virtual ward team use enhanced tracking to ensure that they can reduce the likelihood of admission and, should the patient be admitted into secondary care, follow their process through hospital and attempt to facilitate an earlier discharge back into the community.
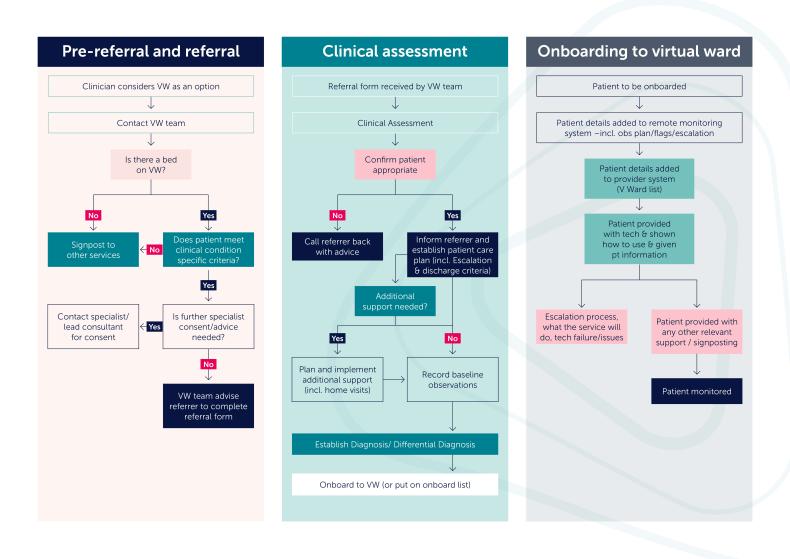
Figure 1: Virtual wards (VW) decision tree
Background
Digital alternatives to face-to-face care can have enormous benefits for both service users and the NHS in managing resources and alleviating pressures on the health and care system. Used well, digital or virtual forms of care are convenient, can be used outside of physical NHS estate and reach more people. Virtual wards are often thought to be a more cost-effective way to deliver care than face-to-face appointments. An evaluation of the Croydon model published in 2021 estimated that the cost saving per virtual ward patient of £742.44 compared to the rapid responses control group. [1]
The use of digital innovations – including virtual wards – that allow patients to receive care remotely help towards early discharge or the avoidance of hospital admission all together, has surged mainly due to their use during the pandemic when face-to-face care was limited and alternative ways of delivering care was
sought.[2] Alongside this acceleration of digital use, faced with the emergency, opportunities for patient consultation were more limited and some normative barriers were removed, including a relaxation of data protection rules in many nations.
The high hopes invested in virtual wards have a longer history. With a backlog of care built up over many years, the pandemic resulted in a halt in elective care in 2020 and 2021, combining to further increase winter pressures on the NHS. In addition, workforce burnout, depletion and increased vacancies – plus recent industrial action – have combined to make reducing waiting times a huge challenge. [3] COVID-19 continues to add to these pressures, with government figures in late March 2023 showing there were just over 7,000 patients with the virus in hospital in England. [4]
The promise of finding solutions to delivering care in a context where face-to-face interactions are being squeezed means much hope has been pinned on the expansion of virtual wards, with more organisations delivering care through various non-physical modes including telecare, remote monitoring, wearable tech and hands-free tech, among others. Furthermore, the increased use of digital technology to provide appointments and services virtually should help reduce unnecessary journeys and air pollution and make an important contribution towards the NHS becoming a net zero carbon health system. A study of three areas published in June 2022 found that as well as costs savings, the use of virtual wards had reduced carbon dioxide (CO2) emissions. [5]
A key principle of virtual care is to release capacity and resource from the wider system and reduce pressure where a bottleneck of high demand and long waits converge to create unprecedented pressure at every point in the system. This is reflected in NHS England’s delivery plan for recovering urgent and emergency care services, published in January 2023. This outlined its ambition to: ‘scale up capacity ahead of next winter to above 10,000 [beds] with a longer-term ambition of reaching 40-50 virtual wards per 100,000 people, which would mean more than 50,000 admissions
a month.’ [6]
According to NHS England there are now more than 340 virtual ward programmes across England, including a total of 7,653 virtual beds. [7] Figures published in March 2023 show that more than 100,000 patients were treated using virtual wards in 2022 and that there had been a 60 per cent rise in virtual beds available between May 2022 and January 2023.8 Virtual wards formed part of the winter plan in 2022 and support the long-term ambition of future
digital transformation for the NHS. This report explores progress and what measures could be taken to help virtual wards fulfil their potential in winter 2023.
Methodology
We undertook one-to-one interviews with a range of NHS leaders including ICS chairs, chief executives, integrated care board (ICB) digital leads, clinicians, and senior operational and finance staff. We also held two ‘deep dive sessions’ which brought together senior NHS and ICB leaders to share their experience of delivering virtual wards within their ICS. In total, 20 people from across all regions, from trust to system level, participated in this work; we are grateful to them for sharing their knowledge and insights. Our questions focused on the following:
- The delivery process of virtual wards.
- The opportunities virtual wards bring to the quality of care and
- impact on demand for the service.
- The challenges leaders face in implementing virtual wards at pace, on time.
- Potential solutions to improving virtual wards, increasing its efficiency and ability to provide an effective pathway for both practitioners and patients.
- The implications virtual wards have for the NHS workforce.
The balance of this report outlines some of the key themes that emerged from this research and goes on to make a number of recommendations, both for NHS England and for those charged with delivering virtual wards.
This research was being undertaken while the Hewitt review of integrated care systems was underway. The review, published in April 2023, considered how the oversight and governance of ICSs can best enable them to succeed, with a focus on getting the balance right on local autonomy and national oversight, and the role of data in driving transparency and improvement across health and social care. Many of the issues covered by the review – and conclusions it comes to – resonate with the experiences, insights and ideas shared by our participants.
An abundance of potential
Among our participants there was considerable enthusiasm for virtual ward expansion. When done well the model is seen as a successful way to keep people out of hospital, discharge early to home, reduce clinical time and give patients autonomy and choice in their own surroundings.
Participants shared positive feedback from patients using virtual wards. Leaders found that providing regular care by a multidisciplinary team gives patients consistent care and expectations of who and when the care is delivered, and that this is being well managed via the virtual ward platforms. Their experience was that managing conditions where a person is living provides a preventative method and allows patients greater control of their care.
The extent of demand for virtual care varies among the leaders we spoke to. However, all agreed that building understanding and credibility among patients is critical to success. In addition, successful pathways were those where patients identified for virtual ward care have been supported through admission by
their clinician.
However, our participants also told us that demand for services and pressure in the system can restrict opportunities for embedding and delivering more virtual care pathways. For example, they shared instances where patients were available and willing to receive care via a virtual ward but where wider social care support was not available. At its best a virtual ward can provide clinical and multidisciplinary support but with more caring elements of human interaction – for example, rest, food and heat – provided at home or in a care setting. Where this human interaction is missing, the unmet need for social care support undermines the potential of virtual clinical care.
Technology alone will not meet demand. The clinicians and leaders we spoke to highlighted the importance of getting the design process right. This includes the methodology for understanding how and why the virtual ward was necessary, as well as access to good data that can both drive demand and identify wider support needs. These factors – alongside collaboration and user-centred design – are needed if virtual ward pathways are to be meticulously planned, to support patients and achieve desired outcomes.
These issues are not new; the NHS has been delivering a form of digitally enabled care – be it telephony or remote monitoring – for many years. However, virtual wards come with a specific set of demands, design and expectations for ICSs, charged with driving their delivery. This requires time and care. Recently published running cost allowance efficiency targets for ICBs will impact on virtual ward delivery. [9]
The recent delivery plan for recovering urgent and emergency care services highlighted how the ‘twindemic’ (of COVID-19 and flu) contributed to record levels of bed occupancy (as high as 95 per cent across England) which, combined with staff burnout, has created a critical bottleneck in hospital capacity. [10] While the potential benefits of virtual wards in helping to address these challenges are clear – there are multiple examples of high-impact implementation leading to reduced length of stay and readmission rates, lower costs and improved patient satisfaction – participants stressed the complexity of implementation.
Case study: Remote monitoring hub in North West region
Borne out of a 2011 partnership between Mersey Care NHS Foundation Trust and Liverpool Clinical Commissioning Group involving 50 patients, the remote monitoring hub, which operates between 8am-8pm 365 days a year, has supported up to around 5,500 people daily to safely manage their health and care at home across clinical pathways including, COPD, heart failure, type 2 diabetes and COVID-19.
Created as a solution to meet specific needs identified through a mix of local and national population health data analysis and risk stratification, the hub’s operation incorporates virtual wards, supports care homes and people with learning disabilities.
Developed through extensive groundwork on strategy and engagement, since 2014 the hub has significantly increased capacity and was able to scale and adapt to challenges, including those resulting from the pandemic, while maximising resources to best support people living longer, often with more comorbidities.
- Since the service began, emergency admissions to hospital among remote-monitored long-term condition patients have consistently reduced by 22.3 per cent on average, compared to those who are not.
- Patient self-reporting suggests a reduction of up to 40 per cent in use of health and care services, including visits to GPs, community nurses and matrons.
- Nursing and clinical teams say the service supports them with effective time management.
- Local teams have increased cross-boundary working across primary, acute and community settings.
- 80 per cent of patients reported increased confidence in managing their long-term conditions.
- Families and friends report they have increased peace of mind.
Data: The area served has a mix of affluent and deprived areas (with a life expectancy variation of up to ten years) and many people living with long-term conditions. Population health data identified cardiovascular disease as particularly prevalent and, along with COPD, a significant cause of death among the
young. The hub was conceived as a new, distinct service to help meet clinical needs of such patients.
Skills: The hub is staffed by professionals in dedicated roles working within the specialist service. These clearly defined responsibilities, now carried out by 30 full-time equivalent staff (including Band 7 specialist nurses and Band 6 tele-health advisers), reflect a now-mature, service-specific structure that supports swift, safe development of capacity and capability. Getting the right skill-mix has been critical to safely increasing the nurse-to-patient ratio from 1:40 to 1:300 for long-term condition monitoring, with additional support to nurses provided by healthcare assistants and administrators. Ensuring staff and patients understand and trust the service through regular engagement and education has been vital to success.
Governance: The hub is underpinned by strong project management and service-specific processes, standards and governance, including performance management metrics and regular reporting. A clinical advisory board supports the development of local pathways, and a remote monitoring programme board focuses on potential benefits and prioritises release of funding, including that provided by NHS England.
Culture: Stakeholder engagement, consistent co-production, educational support and regular evidence-based reporting have all contributed to a significant shift in expectation among health and care professionals and increased confidence among patients. The aim to develop an empowered culture within the
population by instilling confidence and knowledge, encouraging informed condition management outside of hospital and within discussions between patient, professionals, family and friends.
Tools and technology: Patients use an app on their phone or tablet to send information to the hub on their individual health or wellbeing needs, such as vital sign readings like blood pressure or temperature, symptoms of anxiety and depression, or problems with everyday tasks. The hub can provide 4G-enabled devices to patients who do not own one and offers training, regardless of whether people have a personal or NHS device. When a patient inputs their readings, this information reaches the hub via the Docobo digital platform, with intervention rules and pre-set thresholds triggering an alert if a patient’s readings are outside of their personalised ‘normal’ threshold. The team can quickly identify if the patient’s condition is deteriorating and determine the most appropriate course of action, such as increased monitoring or triage.
Source: Merseyside Care NHS Foundation Trust.
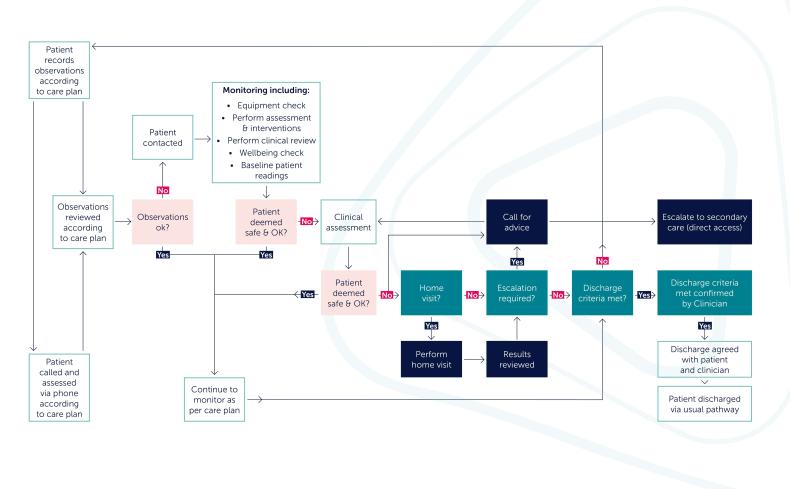
Figure 2: Monitoring on a virtual ward
Implications for the workforce
Integrated care systems – charged with driving the expansion of virtual wards – have yet to be in existence for a year. Each of the 42 differ in size of population coverage, demographics, health inequalities and progress towards embracing and embedding innovative models of working. But while each area is distinct, our research consistently surfaced issues around the challenges facing the workforce, both in availability and recruitment, and how these shape leaders’ ability to deliver virtual wards. This included meeting the target set by NHS England, which is hugely ambitious for some systems.
“Having the workforce in place is a challenge. We need to undertake mass recruitment – at least to train up to 45 members of staff, or capacity is going to run out soon.”
The continuous juxtaposition between supply of available workforce and demand for care throws relentless pressure on the entire NHS. At the height of winter planning in 2022, a major risk identified by NHS leaders was the delay in achieving clinical safety for remote monitoring elements of virtual wards; this had the knock-on impact on the ability to meet the winter target set.
With an NHS workforce vacancy rate of nearly 11 per cent in December 2022 (an increase on the same period a year before), [11] the reality is that the lack of workforce is not only impacting the traditional elements of face-to-face care and impacting waiting lists but is also limiting the ability to harness virtual wards to the full extent expected by NHS England. Again, this challenge is not new; participants told us that before the pandemic, servicing any type of digital care was a challenge for some commissioners due to lack of nurse and clinician availability to lead and absorb the responsibilities virtual wards need.
"The struggle is the workforce. No one wants to take that post [virtual ward] and you need to redeploy from elsewhere”
Currently, the emphasis of virtual ward use is the establishment of at least a frailty and respiratory infection pathway. Where this is working well due to the availability of consultant and senior nurse roles, it is where providers have long-established a model of remote or virtual care before the more recent push from the centre. In these instances, staff resources have been sufficient to allow workforce redistribution to service virtual ward models. However,
participants told us that challenges arise where specialties, such as respiratory and frailty, are dictated as this results in a smaller recruitment pool, especially in the context of NHS workload overwork, burnout and low morale at all levels.
“As a system the workforce is the biggest constraint… recruiting is hard. Workforce has grown but not in activity; [this] might be relieved if we get the balance right of workforce to activity but that is difficult right now.”
Participants stressed that these workforce challenges are continuing to impact across the whole of the NHS and are hindering the ability of virtual wards to make rapid and effective progress. They emphasised that there was strong enthusiasm among clinicians and providers for virtual wards, for using technology and identifying suitable patients.
Participants also highlighted that the specific skill set and career pathway needed for virtual wards remains a significant barrier. In overcoming this, they felt that a more effective model was needed that would have in-built flexibility across specialties or clinical teams who are able to work across pathways and within multidisciplinary teams, with the ability to pivot and call in specialists if patients’ needs escalate. Such an approach to virtual wards – supported by NHS England – would need to use a flexible approach to recruiting staff and be less tied in with specialities.
“Our main challenge is not having enough staff even for seven-day cover, no cover for band 2 [nurses] and recruiting band 2 or 3 has been very hard.”
The assumption made is that delivering a digital model of care means fewer NHS staff as fewer face-to-face touch points are created. However, to deliver the model, clinicians are required to drive the virtual ward forward with enthusiasm, leadership and full accountability. Participants highlighted the importance of consultant enthusiasm as a critical driver to successful implementation of virtual wards. However, they also said many consultants are concerned about absorbing the full risk of managing and discharging patients in this way. In alleviating this concern, participants said building staff confidence is vital. Their experiences show that supporting clinicians at all levels with risk stratification, discrepancy, confidence, education and training, helps to shift the mindset of those who are yet to be sold on the value that virtual wards can bring to their speciality and to patients.
“Virtual wards are dependent on the clinician to take the case on and rebadge their complexity for high-level decision-making and what the hospital admission is likely to offer.”
Three ICS virtual ward leaders we spoke to told us about peer-to-peer senior consultant engagement and the desire to replicate colleagues’ virtual ward success once noticeable changes have been seen and risks mitigated. Having digital and ‘virtual ward champions’ in place, whose role it is to spread awareness across the hospital and – more importantly – across the multidisciplinary and integrated care pathway, made a significant impact in how
quickly and effectively a virtual ward had been set up. Participants’ experiences suggest that the good will and ability of champions – where senior clinicians and consultants fully lead virtual wards and have a long-term investment in their success – are critical but challenging to operationalise.
Overcoming these challenges involves raising clinical and operational awareness of virtual wards through investing in engagement. Participants reported that working with clinicians and engaging patients in co-design from the start of the pathway design process contributed to success. Harnessing the opportunity for clinical transformation, designing and changing pathways and principles to meet the demands of the NHS and the opportunity to scale innovation, were key drivers of successful virtual wards.
Faced with reduced staff and high demand, where leaders and clinicians worked in partnership to employ risk-stratification strategies – including redeploying staff and onboarding tools for virtual ward pathways – significant gains in developing and governing virtual wards were made. Indeed, many of these gains were made during the pandemic when providers worked quickly across boundaries, teams and organisations to share resource, skill and risk to scale virtual services. For example, where telehealth was being delivered during the pandemic, where systems and governance were already in place, these were more easily tweaked and directed towards the development of virtual wards.
Participants told us that staffing challenges were further exacerbated where specialist nurses are still needed for taking the responsibility for discharging patients. Although in the virtual ward pathways the monitoring is remote, clinicians are reluctant to take the responsibility to discharge a patient unless a face-to-face visit has been carried out or where senior consultants have been involved in the care and are willing to discharge.
Even where virtual ward roles are advertised as remote working, for those providers in a rural setting, the lower band staff are not attracted to that location or provider, further exacerbating workforce challenges. Conversely some leaders, especially those servicing a city population, said that previously retired clinicians were attracted to the virtual ward roles as demand was manageable and home working since the pandemic was attractive.
Case study: Heart failure virtual ward
Colette Melia, 66, whose formidable experience in the telehealth virtual ward, demonstrates the service’s clinical significance and the scope of virtual wards in improving the quality of life and patient experience.
Colette regularly visited the hospital, as the former university law lecturer had been forced into early retirement following her diagnosis of Crohn’s disease, affecting the digestive system. After nine years of unexplained breathlessness, she was diagnosed with heart failure. This left Colette despondent and weary of making the trips to the hospital. The uncertainty about when she needed to go to the hospital posed a significant mental strain on Colette, and her anxiety heightened within her personal life, as her quality of life depreciated.
Colette was referred to the telehealth heart failure virtual ward by cardiologists, as she met the suitability criteria for virtual ward admission. She has been triaged by telehealth clinicians, admitted to the ward, and delivered the equipment to her home: a smart device, blood pressure monitor, pulse oximeter, scales, a thermometer, and a pedometer.
She was trained to record vital signs and symptoms daily and enter them into a smart device, sending them to a safe monitoring platform called Docobo. The nurse clinicians in the telehealth clinical hub monitored vital signs and alerts and then completed a telephone consultation with Colette to assess for early deterioration of her symptoms, which would be escalated to the consultant cardiologist on the daily virtual ward round.
Colette remarked, “I was apprehensive about using the equipment, but it’s simple. It’s just like being on a ward; you’ll get an immediate response which is very reassuring. They have a virtual ward round like in the hospital, so I know my readings can be reviewed by a cardiologist as if I were on an actual ward.”
Colette had severe heart failure and required a biventricular pacemaker. Her treatment was optimised in the virtual ward and prevented hospital admission while waiting for the pacemaker. Colette’s vital signs stabilised after a week and her pacemaker procedure as was done as a day case, all while staying in the virtual ward. Post procedure, Colette developed complications, and her heart rate dropped due to failed pacemaker settings and irregular heart rate. The nurse clinicians promptly identified the complication by reviewing the clinical readings and arranged a planned admission to the pacemaker clinic. This prevented potential complications of heart block and emergency hospital admission by providing timely and quality care.
Colette was discharged from the virtual ward post optimisation of treatment, and stepped down from the virtual ward to long-term condition monitoring for continuity of care. Colette said: “It’s perfect. You know they’re there, watching your readings, which gives you the confidence to get on with your life. I was so worried that I couldn’t concentrate on anything. I feel like I’ve got my life back.”
Designing the care pathway
“Ideally the centre would own innovation and best practice while locally we will collate the interesting examples, undertake reviews and evaluations and work out locally what best practice suits that can be adopted. The local leadership team should monitor implementation locally and, if needed, call on regional teams for support.”
For patients and communities, the initial tangible difference in receiving care through a virtual ward is the use of digital technology in place of human interaction. While one of the benefits for providers in delivering care virtually is the potential to reduce clinician time and to alleviate pressure on demand and redeploy staff, the technology being used across providers and systems varies. Each ICS is on its own digital maturity journey, with some further ahead than others. While the need to have a digital strategy is outlined in What Good Looks Like, the reality is that some ICSs will have further developed and implemented their strategy than others. [12]
“Technology is important, but processes need to be right. How do we get medicines to the patient if the hospital doesn’t have [an] electronic prescribing system? All good and well delivering pathways but the infrastructure is not there in first place.”
Participants felt that the current focus on availability of technology and admission avoidance is not enough on its own without the use of good available data to understand where prevention opportunities lie. They stressed that designing the care pathway now and for the future needed to be based on fully understanding demand and that this required access to good data that can shape priorities for improving patient outcomes, evidence prevention in the population and free up bed capacity and financial efficiencies.
"Elderly [patients], the best place for them is at home. But it is hard to provide the same level of care from hospital in the community. In the ward you can get medicines within hours, in the community chances are that there is a practical delay and lag for the meds.”
Combined, these factors should be the driving force behind how quickly and concertedly virtual wards can be set up. In addition, if patients and communities are to be targeted in the hope of reducing or avoiding hospital admissions through clear data and evidence, they also need support and care to stay well outside of the hospital; this issue can be supported by technology but goes much wider; people also need reassurance, advice and care which is provided by human interaction.
Participants reported that very often targets set nationally become the main driver for setting up virtual wards, without giving local leaders the ability and autonomy to lead the methodology and design of the care pathway. The resulting risk is that virtual wards are driven by secondary care demand rather than what can be safely achieved. It is crucial that what drives a virtual care pathway is a design and methodology informed by deep understanding of the risk profile and what is needed from a population health perspective.
Currently the NHS lacks the full knowledge and information about the future health modelling and the risks facing our populations and communities. Without this it is not possible to fully understand risk factors, to appropriately manage those scenarios and needs in the longer-term, or to shape what those needs may look like across a whole integrated health and social care pathway.
These issues lie at the heart of the Hewitt review that makes a number of recommendations, including: [13]
- fewer central targets to enable systems to prioritise how they use their resources based on the needs of their local populations
- making data held by NHS England about performance available to ICSs themselves.
Local autonomy and national prescription
In winter 2022, the NHS faced crippling pressures across every part of the service. Challenges, including timely access to urgent and emergency care and ambulance handover delays, were at their highest level coming into a winter. The discharge of patients impacted on patient flow within hospital, accompanied by sustained demand for primary care services and pressures in mental health services.
To address some of these capacity challenges, NHS England requested 7,000 additional general and acute beds, through a mix of new physical beds and scaling up virtual wards. [14] In April 2023, NHS England released data which showed that in March 2023 this target was met, with an additional 7,820 beds being made available of which 628 were virtual beds. [15] While this increased capacity is welcome news, it is unclear how the NHS fared over the rest of winter with bed capacity and whether virtual wards bed were available at a similar, consistent rate over the entire period.
“The current definition doesn’t take into account other work that is ongoing across specialities and pathways. It misses the opportunity to care for others not in hospital and needs to be wrapped around social care. It feels like it’s a case of hitting the target and missing the point.”
As noted above, currently, NHS England dictates that the focus of virtual wards are on two pathways: frailty and respiratory. Participants of this research told us that a more effective model would be to give more control to integrated local care leadership teams, with ICSs monitoring local population needs and demand through accurate and available data modelling. This collection of local data should be used to make bespoke, local healthcare decisions that address the needs of that population in every ICS. Leaders felt that a more workable model would involve NHS England focused on driving innovation and best practice, while allowing local systems to deliver and monitor the virtual wards specialty which reflects its population health needs.
Participants felt that the current definition of virtual wards is too prescriptive and too narrow in scope and that a more flexible approach is needed to encourage and harness virtual care in other areas of NHS care beyond acute care, including mental health, primary and community care. This less rigid approach would need be informed by the wider social care gap that impacts on a wider range of patients outside hospital settings.
To be truly impactful for quality of care and productivity through efficiencies gained, virtual wards should be approached as a coherent much larger-scale initiative, accepted and treated as a holistic digital project. This requires striking the right balance between local autonomy and national responsiveness and oversight.
Funding approaches
For 2022/23 and 2023/24, £200 million of funding was made available from the Service Development Fund (SDF) in 2022/23, with an agreement that a further contribution of £250 million – on a match-funded basis – will be available in 2023/24.16 The process set out that this temporary funding will support the establishment of virtual wards; however from 2024/25 systems will need to ensure virtual wards are built into their long-term strategy and financial plans.
"[The] match-funding process makes decisions harder and really unhelpful. The way the funding is structured is a risk so we cannot fund posts like project manager. It’s all slow to appear and we cannot make plans.”
The leaders involved in this research explained that the initial delay in funding to reach systems had a significant impact on setting up and initiating virtual wards. The delay in receiving funding from availability to receipt, which was up to ten weeks in some cases, risked destabilising the pathway and had the knock-on effect of not securing clinical capacity and buy-in and the loss of staff.
When funding is structured into short-term streams, it perpetuates a cycle of short-term chaotic commissioning and prevents long-term fully integrated service design that has the ability to return quality of care and productive outcomes. Participants told us about how this increased the risks associated with commissioning virtual wards. For example, funding for posts such as a programme manager to oversee the implementation of virtual wards is currently not available for more than 12 months and this acted as a barrier to planning ahead. Furthermore, reporting strong outcome measures over a short timeframe does not show the full benefits of virtual wards. Conversely, when systems have the evidence and evaluation to show the longer-term impact of certain innovations, they do not have the funding flexibility to make those long-term commitments.
Investment in virtual wards need to be long-term and flexible. This would help to strike the right balance and bring clarity to the issue outlined earlier around local responsibilities, autonomy and national oversight. While the Hewitt review does not go into detail on virtual wards, it does recommend that the government and NHS England end the use of small in-year funding pots with extensive reporting requirements for the NHS and social care. The review also concludes that NHS England should give ICSs more flexibility to determine allocations for services and appropriate payment mechanisms within system boundaries and that the government should increase funding and attention aimed at enabling a shift towards upstream investment in prevention.
Viewpoint and recommendations
While this research involves a selection of those involved in the delivery of virtual wards, what was striking was the consensus that emerged, both in participants’ commitment and enthusiasm for expansion as well as the challenges they face. At the heart of this are two related areas of challenge.
The first is, for some, finding the time and space to put this enthusiasm into practice in the current context of severe pressures facing the NHS and its workforce. While these pressures make realising the potential of virtual wards more important and urgent, participants were clear that change should also be driven by prevention and patient safety. As we have seen, success depends on deep and time-consuming groundwork to be done at the pathway design phase, including engagement with clinicians and patients to build confidence and trust.
The second area involved a range of tensions that speak to many of the issues addressed by the Hewitt review and speak to the fact that for many decades the constituent parts of the NHS have been asking for the ability to be trusted, empowered and make decisions on behalf of their population, which they know best. The review sets out six key principles for creating the context in which ICSs can thrive and deliver:
- collaboration
- a limited number of shared priorities
- giving local leaders space and time to lead
- providing systems with the right support
- balancing freedom with accountability
- enabling timely, relevant, high-quality and transparent data.
More specifically, our participant discussions suggest a number of recommendations that either overlap with the Hewitt review’s conclusions and/or are specific to effective, safe and welcome virtual wards expansion.
Government, NHS England and policymakers
- To be truly impactful on both patients’ quality of care and NHS productivity, it must be recognised that there is a severe workforce and skills shortage in the NHS which is impacting on systems’ ability to fully develop, deliver and scale the full ambition of virtual wards. While we await both the national workforce plan and the digital, data and technology workforce plan, it cannot be underestimated how this steady lack of available workforce over the years continues to affect the feasibility of delivering virtual wards at scale.
- Currently, the emphasis of virtual ward use is the establishment of at least a frailty and respiratory infection pathway. The definition of virtual wards needs to be less prescriptive and enable a more flexible approach to encourage and harness virtual care in other areas of NHS care beyond acute care, including mental health, primary and community care. This less rigid approach would need be informed by the wider social care gap that impacts on a wider range of patients outside hospital settings.
- NHS England should focus on driving innovation and best practice in virtual wards, while allowing local systems greater flexibility to deliver and monitor models that reflects its population health needs.
- Local data should be used to make bespoke, local healthcare decisions that address the needs of that population in every ICS. Currently the potential for increasing effective use of virtual wards is undermined by lack of access to good data on local population needs and demands. This data must be made available by NHS England so that systems can make the appropriate local decisions.
- Investment in virtual wards need to be long-term and flexible. In addition, social care funding support must be available. At the moment, short-term funding models are hindering recruitment, planning and impact assessment. In addition, the absence of adequate funding for social care is preventing systems from fully addressing the holistic and wrap-around needs of patients away from only clinical virtual ward support.
For local leaders and integrated care systems
- To realise the full potential for communities and deliver on NHS productivity, virtual wards should be approached as a coherent larger-scale and holistic digital project. There is considerable enthusiasm among clinicians and local health leaders for increasing the use of virtual wards whose experience showed that when done well, they can help keep people out of hospital, discharge patients early, reduce clinical time and give patients autonomy and choice.
- ICS leaders should promote the use of ‘virtual ward champions’ to spread awareness across secondary care, multidisciplinary and integrated care pathways as well as raise awareness of the model among patients and communities. Our participants found that this was an effective way of marshalling the good will and ability of senior clinicians and consultants who have a long-term investment in their success.
For clinicians, staff and communities
- In implementing new virtual wards, clinicians, leaders and communities must be involved in co-design from the start of the design process. Successful examples of virtual wards have depended on patients identified for virtual ward by fully engaged and enthusiastic senior clinicians supporting the ambitions of the virtual wards programme. Patients and communities should feel empowered to discuss alternative means of receiving care with their clinicians and discuss the possibility of virtual care within a care pathway.
There has been a significant increase in the development and establishment of virtual wards over recent years. While this innovative care model provides flexibility, better use of technology and manages demand capacity, we must be realistic about what the model can achieve within the NHS.
With the current workforce shortages and rising demand for care, virtual wards can only be successfully delivered by a fit-for-purpose workforce that is in place over a longer period of time. System leaders need the right balance of support and empowerment to design and deliver virtual care services which address the demand capacity specific to their population health needs.
References
1. Health Innovation Network South London (2021), Rapid Evaluation of Croydon Virtual Ward.
2. Nuffield Trust (2020), The remote care revolution during Covid-19.
3. NHS England, “NHS cuts waiting lists as A&E departments busier than ever before”. 12 January 2023.
4. Gov.UK, Coronavirus (Covid-19) in the UK. 6 April 2023.
5. Romanello M. Guest post: Calculating the carbon footprint of the NHS in England. CarbonBrief
Clear on Climate. 2021
6. NHS England (2023), 2023/24 Priorities and Operational Planning Guidance.
7. NHS England, ‘World-leading NHS virtual wards treat 100,000 patients in a year’. March 2023.
8. Ibid.
9. NHS Digital (2023), NHS Vacancy Statistics, April 2015-December 2022, Experimental Statistics.
10. NHS England (2023), Delivery Plan for Recovery of Urgent and Emergency Care.
11. NHS Digital (2023), NHS Vacancy Statistics, April 2015-December 2022, Experimental Statistics.
12. NHS England (2021), What Good Looks Like framework, first published 31 August 2021.
13. Department of Health and Social Care (2023), Hewitt Review: an independent review of integrated care systems.
14. NHS England (2022), Next steps in increasing capacity and operational resilience in urgent and emergency care ahead of winter.
15. NHS England, NHS progress on waiting list despite busiest winter on record. April 2023
16. Department of Health and Social Care, Up to £250 million to speed up hospital discharge. 9 January 2023.
About us
NHS Confederation
The NHS Confederation is the membership organisation that brings together, supports and speaks for the whole healthcare system in England, Wales and Northern Ireland. The members we represent employ 1.5 million staff, care for more than 1 million patients a day and control £150 billion of public expenditure. We promote collaboration and partnership working as the key to improving population health, delivering high-quality care and reducing
health inequalities.
For more information visit www.nhsconfed.org

Acacium Group
Acacium Group is a leading global healthcare delivery partner. With over 35 years of experience and 24 specialist businesses, we improve people’s lives through expert healthcare, social care and life sciences. By combining access to workforce, technology and sector expertise, we increase the sustainability of the global healthcare system, from early-stage clinical research right through to palliative care.
For more information visit www.acaciumgroup.com.
About this report
The work for this project was supported by Acacium Group. This output was independently developed, researched and written by the NHS Confederation, with input from Acacium Group.



