Patient-initiated follow up: designing it with patients at the centre
Key points
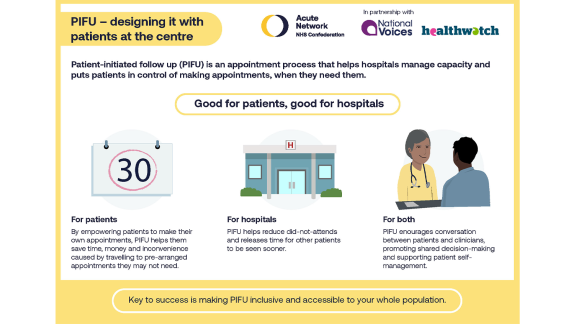
The elective care backlog is an ongoing challenge for services and has meant the NHS has had to look for ways to better match clinical resources with demand and reduce patient waiting times. Patient-initiated follow up (PIFU) has been given a renewed focus as a potential way to help reduce this backlog by better managing outpatient follow-up appointments while also giving patients greater flexibility and control over their care.
PIFU encourages conversations between patients and clinicians, supporting patient self-management and promoting shared decision-making. At a time when services are challenged matching clinical resources with demand, PIFU looks to benefit both patients and providers, freeing up valuable capacity and improving patient access and satisfaction.
As PIFU is scaled up across the NHS, with many trusts looking to establish their own services, it remains important to look at considerations beyond healthcare to ensure services are appropriate and equitable for all patients using them.
To address any potential inequalities around PIFU, this briefing highlights three key areas of the service to consider in making PIFU inclusive and accessible to the whole population.

Find out how to design a patient-initiated follow up (PIFU) appointment process that is inclusive and addresses health inequalities.
Background
At the beginning of 2023, Prime Minister Rishi Sunak delivered a speech setting out five priorities, with one of the pledges being to “cut waiting lists” in the NHS. While long waiting lists are not new, with pre-pandemic waiting lists for care already at 4.43 million in February 2020, latest figures in April 2023 show record numbers of around 7.42 million people are waiting for treatment.
In outpatient care, figures from across England in 2021/22 show that the total number of appointments has increased by only over one-third from a decade ago to 122.3 million with just over half of these appointments accounting for follow ups. As the demand for services continues against the backdrop of the growing elective waiting list, there is an increasing challenge to match the needs of patients with the clinical resources available.
PIFU, which encompasses terms such as open-access appointments, self-managed follow up and see-on-symptom appointments, has gained renewed attention as a model of follow-up care. It was at the forefront of last year’s elective recovery guidance, where a goal was set to reduce outpatient follow ups by at least 25 per cent and expand the uptake of PIFU pathways to 5 per cent of outpatient attendances by March 2023, and remains among this year’s elective care priorities.
PIFU pathways
In traditional care models, patients who have had treatment or surgery, or suffer with chronic conditions are provided with a set care plan and offered scheduled follow-up appointments either conducted in person, or remotely. PIFU offers an alternative way of organising planned follow-up care for patients following their elective procedures, rather than automatically being scheduled for appointments. This aims to give greater control to patients over the timing of their follow-up appointment based on their health status needs, helping patients save time, money and the inconvenience of travelling to pre-arranged appointments they may not need.
Susan Buckley at Derbyshire Community Health Services NHS Foundation Trust, who oversees the PIFU service at the trust's outpatient physiotherapy service, outlined to us that their PIFU service was about:
“putting patients at the heart of it and making those decisions themselves”
As part of a national discussion taking place across the NHS, there has been focus around a shifting service model, one that better serves the needs of patients and the communities they live in. Recently, Matthew Taylor, chief executive of the NHS Confederation, has discussed the idea of a future service model that is centred around “empowering and enabling patients and communities to improve their health and wellbeing”, representing a new social contract between the NHS and public.
PIFU, which looks to give greater control to patients, embodies this idea of patients being more involved in their own care. Evidence suggests that by allowing patients greater freedom over the timing of their follow-up appointment, based on their individual health status needs, there is greater patient and clinical satisfaction.
Helping patients to manage themselves
Equally, while it remains difficult to truly measure the extent of PIFU’s impact alone on the elective landscape, giving patients the ability to decide when they require follow-up care has the potential to improve wider operational services. Susan described that PIFU has enabled patients to manage themselves and arrange appointments only when they need to, potentially reducing unnecessary appointments and decreasing the number of missed or cancelled appointments. This has enabled the physiotherapy service to better prioritise patients needing assessment who had not yet been screened for red flags.
PIFU encourages conversations between patients and clinicians, supporting patient self-management and promoting shared decision-making. At a time when services are challenged matching clinical resources with demand, PIFU looks to benefit both patients and providers, freeing up valuable capacity and improving patient access and satisfaction. However, it is important to ensure the decision-making around patients being moved onto PIFU is a shared conversation with an agreed outcome. There is a concern that ambitious figures like the 25 per cent reduction in follow-up attendances could lead to providers driving towards outcomes that do not work for patients. Involving patients and ensuring shared decision-making as part of a patient-centred shift alongside ambitious targets will be key towards transforming patient outcomes across PIFU services.
Making PIFU inclusive
When redesigning services, there is always a risk of exacerbating existing health inequalities. As PIFU looks to be scaled up across the NHS, with many trusts looking to establish their own services, it remains important to look at the considerations beyond healthcare and ensure PIFU is appropriate and equitable for all patients using the services.
To address any potential inequalities around PIFU, we have highlighted three key areas of the service as important to consider in making PIFU inclusive and accessible to the whole population. They are centred around:
- Assessment
- Consultation
- Supporting information
Assessment
While PIFU should be accessible and available to as many of the population as possible, there is an important process between the clinician and the patient to determine the appropriateness of PIFU for each individual patient. After discussing this assessment process with an operational leader, they affirmed that risk management is essential during this process, outlining that services must be clear on their criteria, to identify who is or isn’t appropriate to be included in the framework. Building the following considerations into the assessment process and service design may help assess the individual effectiveness of PIFU for each patient.
Cultural, economic and social differences
There are cultural, economic, and social differences among patients. These can impact perceptions of health and beliefs around the causes and treatment of diseases. They can also impact how pain is expressed or experienced and how people might seek help. PIFU must be respective and responsive to diverse needs. It must also try to balance the medical model with risks from cultural variation.
Vulnerability or anxiety
Some patients might feel vulnerable or anxious which could make them feel less confident in initiating a follow up. Some symptoms might be seen as embarrassing for some patients. It is vital they feel welcomed, comfortable and safe in managing their conditions. Equally, healthcare is not just about managing the medical condition, it’s about managing patient concerns, queries, and anxieties. Considerations of wider needs that are often addressed in scheduled appointments still need to be met when patients are under PIFU. This is where the accessibility for patients on PIFU services is important.
Accessibility
For patients to address their concerns and receive the follow-up care they need, ensuring appropriate, access for all patients on the PIFU service is vital. For example, 6 per cent of homes (1.5 million people) do not have access to the internet and some do not have access to phones or computers. Access also might be restricted by opening hours and long waiting queues. Ways to access PIFU therefore need to be flexible, whether that be by providing online, phone or drop-in service channels. PIFU also needs to be easy to navigate and set up new appointments. For this to happen, services need to be tailored to meet specific patient needs.
In addition to addressing digital exclusion, it is also important to consider socio-economic factors when addressing access issues. Research from Accurx found that individuals from disadvantaged groups were much more likely to forget their appointment. Finding that approximately 12 per cent of patients admitted to forgetting their appointments, with this response being more prevalent among disadvantaged groups. This was partly attributed to the limited resources and complex circumstances that individuals from disadvantaged backgrounds often face.
These findings around ‘Did Not Attends’ (DNA) raises an important point around how this would likely play out in PIFU. Some individuals, particularly those who struggle or are unable to prioritise their health, might not be suitable for PIFU.
Safeguarding
There might be challenging personal circumstances that can make it difficult for patients to engage with PIFU. It is important to consider the safeguarding issues during the assessment criteria. Personal circumstances for patients, such as relationships and power imbalances at home, can make it difficult for some patients to take ownership of their own care needs. The level of vulnerability must be taken into consideration when assessing a patient’s suitability for PIFU.
However, there is an acknowledgement that trying to assess and pick up every consideration is extremely difficult. This was acknowledged by Susan Buckley, and to address this in their service and help clinicians with assessment decisions, they implemented a standard operating assessment procedure that was drawn up with NHS England’s PIFU inclusion criteria.
Consultation
Once patients are admitted onto a PIFU service, engagement with the patient and gathering feedback is an important step in ensuring services are continually responsive to the diverse needs of its patients. Susan Buckley highlighted the importance of patient engagement, describing it as important to continually improve the accessibility and outcomes for patients that are on their PIFU service, to help facilitate and shape further changes to services.
When undergoing these consultations, understanding how patients find the way they access PIFU could be valuable towards making it more accessible to those who are already using the service, or potentially will be. Another important area of focus is around the ease in which patients feel they can use the service; PIFU should be an easy process for both clinicians and staff when describing symptoms and choosing a follow-up date. Equally, how PIFU is presented could also be an important area for feedback, so clinicians are able to understand how patients would best prefer the information to be presented.
This consultation process can help shape the experience of the assessment process from a diverse range of patients who are on the PIFU programme and can be used to further refine the service itself to better fit the patients who use it.
Supporting information
When introducing a PIFU service to patients and carers, explaining exactly what PIFU is and how it works is important for both clinician and patient buy-in during the shared decision-making process. Together with accompanying patient information, patients and carers should feel confident to decide when they need an appointment and also feel assured they can easily arrange one, when necessary.
...it is helpful that the content is in a style that is accessible and in different formats that meet the needs of diverse patient groups
However, patient organisations have highlighted that the term 'PIFU' means nothing to patients, even if described as patient initiated follow-up. It is important that the content and communication around PIFU is centred around patient understanding. This was identified as a key area by Susan, outlining the importance of clearly explaining the benefits PIFU can offer patients and improving patient understanding that it is not simply a tool to manage waiting lists. For the physiotherapy service,
it was an important step towards getting patients to understand PIFU as a service and to reassure them they are not just being removed from the list. To achieve this, they developed ‘preparing for your appointment’ leaflets and published information on their website. This information supports patients to understand exactly what PIFU is, understand that it is an option, and understand the benefit to them.
When looking to provide supporting information alongside the PIFU service, it is helpful that the content is in a style that is accessible and in different formats that meet the needs of diverse patient groups. We have heard it is helpful to patients if it is written in language avoiding acronyms and technical words, available in languages that fit population demographics. The language should also suit the needs of those who, for example, have cognitive, visual, or hearing impairment to ensure patient re-engagement is accessible and in line with the conditions set out in the Accessible Information Standard, a new set of guidance due to be published this autumn.
PIFU aims to give patients:
- greater control over their own care
- reduce unnecessary appointments
- decrease the number of missed or cancelled appointments
- improve patient experience and satisfaction.
It also looks to benefit services:
- giving clinicians more time to prioritise patients on the waiting list who need to be seen
- helping to reduce patient waiting times
- manage the elective care backlogs.
However, to empower patients to take greater control of their own care, it means shaping a service that is easily accessible, flexible, and adaptive to their individual needs. While PIFU won’t be appropriate for all patients, for those who are part of a PIFU service, a continued drive to adopt patient feedback and provide clear communication channels to support them is key in trying to reduce the health inequalities that exist or could potentially arise.
Supporting material
To support developing successful and inclusive PIFU processes, we have:
- produced an infographic
- published a case study with three examples of how using PIFU has reduced unnecessary outpatients appointments, overdue referrals and waiting lists through patient-initiated follow up.