Integrated care systems (ICS): parliamentary briefing
Key points
- The Health and Care Act was passed in April 2022. The legislation puts integrated care systems (ICS) – which have existed in shadow form for a number of years – on a statutory footing from 1 July 2022, meaning they are now responsible for planning and funding health and care services in the area they cover.
- They are a core part of the NHS Long Term Plan from 2019 and build on how services have been working together already at local levels to orientate health and care much more around the people they serve rather than their organisational boundaries. Their establishment represents the first large-scale structural change to the NHS since 2012.
- Integrated care systems (ICSs) are partnerships that bring together the health and care organisations in a particular local area, to improve population health and healthcare, tackle unequal outcomes and access, enhance productivity and value for money and help the NHS to support broader social and economic development.
What are integrated care systems?
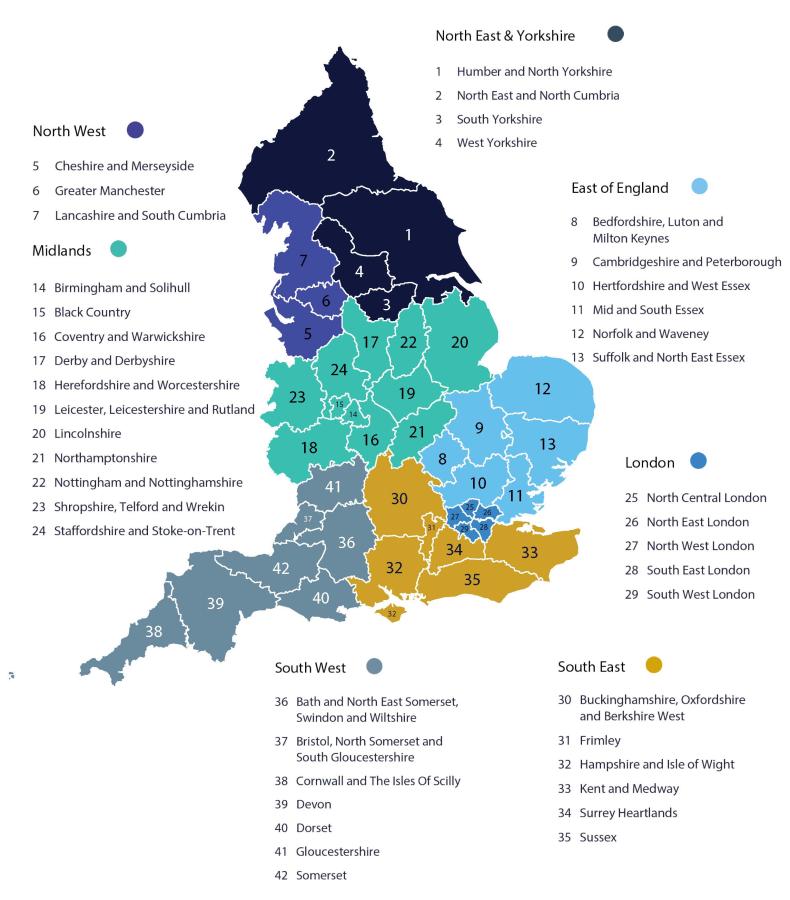
Integrated care systems (ICSs) are partnerships that bring together the health and care organisations in a particular local area, serving anywhere between 600,000 and million people, to work together more closely and provide joined-up care. The 42 integrated care systems replace the now dissolved 106 NHS clinical commissioning groups (CCGs) that came before them and lead on funding and planning healthcare services in their local areas.
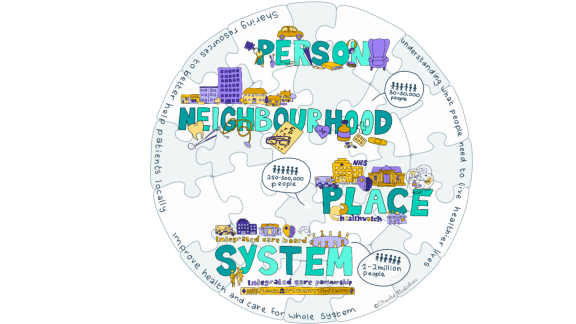
Each ICS is made up of an integrated care board (ICB) and an integrated care partnership (ICP):
- The ICB is responsible for planning NHS services, including ambulances, primary care, mental healthcare, hospital (acute), community and specialist care. They have both a chief executive and chair, and they are accountable to NHS England for NHS spending and performance within their boundaries.
- The ICP has a broader focus, covering public health, social care and wider issues impacting the health and wellbeing of their local populations. t operates as a statutory committee between the ICB and each of the local authorities in the ICS geography, as well as voluntary, community and social enterprise (VCSE) organisations, care providers and other key partners. Exact membership is determined locally.
How will integrated care systems work?
There are 42 ICSs across England. All 42 ICSs have been established with four strategic purposes:
- Improving population health and healthcare
- Tackling unequal outcomes and access
- Enhancing productivity and value for money
- Helping the NHS to support broader social and economic development
These strategic purposes have been agreed because our health is affected by many things – housing, unemployment, financial stress, domestic abuse and poverty. This is something that we need to look at through a partnership between the NHS, local government and the voluntary sector.
ICSs will help deliver more joined-up and better care for the public by bringing councils, voluntary and community services and the health service together in a particular area.
ICSs will focus on delivering care at a ‘place level’. This means bringing together all the health and care organisations to form place-based partnerships including council-run health and wellbeing boards and all health and care organisations sitting within a place-based area of around 250,000-500,000 people. The knowledge these organisations have of local people’s needs means they can work together to make sure services meet the needs of the people who live within that place.
Below the place level, services will be delivered at neighbourhood levels of 30-50,000 people, usually corresponding to an electoral ward or district of a borough council. They are served by groups of GP practices working with NHS community services, social care and other providers to deliver more coordinated care, including through primary care networks (PCNs).
What do integrated care systems mean for your constituents?
This will, in part, be down to the work your local ICS has already been doing in shadow form over the previous few years. There is a degree to which the Health and Care Act is formalising in law the ways of working that are already happening and the legislation has been drafted in a way to allow them to develop in their own way.
ICSs are intentionally varied as different local populations have different health and care needs.
For many of your constituents, the changes will not be obvious straight away – they will continue to access care from the usual providers. Over time, the care delivered to patients will become more joined-up, with fewer barriers to care and a greater emphasis will be put on prevention and improving population health. In the medium to long term, this will improve health outcomes in local populations, reduce health inequalities and reduce pressure on hospitals.
Why do we need integrated care systems now?
Many areas of the country are already working in integrated ways, but their progress has been stymied without statutory powers and duties. Over the course of the pandemic, many health and care organisations worked together well to deliver care in the face of a public crisis and it’s critical we harness this now.
ICSs becoming formalised on 1 July is an important next step in a longer-term process.
The NHS is facing unprecedented challenges with the elective backlog, increased pressure on mental health, primary care and community services, the ongoing threat of coronavirus and a growing cost of living crisis, against a backdrop of 105,000 staff vacancies and years of underinvestment in capital.
ICSs will be a key part of helping the NHS understand and respond to these challenges at local levels, supporting people to get more personalised care and ensuring that public expenditure in the NHS is put to best use.



