Community-based glaucoma monitoring services

Overview
To address rising demand and capacity challenges in secondary care, Primary Eyecare Services, a clinically led, not-for-profit provider, pioneered a community-based Glaucoma Monitoring Service. The service supports NHS goals by shifting care from hospitals to neighbourhoods, embracing digital innovation and prioritising prevention.
What the organisation faced
Glaucoma is the leading cause of irreversible sight loss in the UK, affecting over 700,000 people, with nearly half undiagnosed due to its symptomless progression and long hospital waiting times.
The NHS has been confronted with hospital waiting times for glaucoma that can reach up to 72 weeks in some areas. The NHS faces a 25% rise in major eye conditions between 2022–2032, outpacing population growth sevenfold.
The rising demand has led to secondary care glaucoma services struggling to manage capacity across England, there is a need to reduce unnecessary hospital referrals and patient travel and to improve early detection and management of glaucoma.
The improvement
To address these challenges, a community-based Glaucoma Monitoring Service was developed and is now operating in 10 NHS areas. Community optometrists monitor low-risk glaucoma cases under a structured management plan, using the GLAU-STRAT-FAST risk stratification tool.
Examinations include patient history, visual acuity, intra-ocular pressure, visual fields, anterior chamber assessment, optic nerve head assessment and OCT imaging.
Following consultation, patients may continue to be monitored in the community, be discharged to routine sight testing or be referred back to secondary care if necessary.
The service model has evolved to allow independent monitoring of low-risk cases with mechanisms in place for returning patients to hospital care as needed, such as web-based virtual reviews or direct clinical document delivery. Notably, pilots in Mid and South Essex and Greater Manchester have demonstrated effective collaboration between primary and secondary care.
Outcomes
An analysis of 515 patient episodes in community glaucoma services showed 5.4% were discharged, 8% were referred back for specialist care, 86.6% remained in community review.
Of those remaining, 83.2% were placed on a 12-month recall or longer and 16.8% on a 9-month or shorter recall. As a result, 98.3% would recommend the service, and 88.9% rated their experience as six or seven out of seven (Seven being the highest rating or ‘Excellent’).
Overall, the monitoring services are well-received by patients, safe and effective, and show strong agreement between primary and secondary care. They reduce unnecessary hospital referrals, cut patient travel and offer a scalable, sustainable model for integrated glaucoma care. Wider and more consistent commissioning across England could further enhanced access, efficiency and outcomes in glaucoma care.
Mid and South Essex
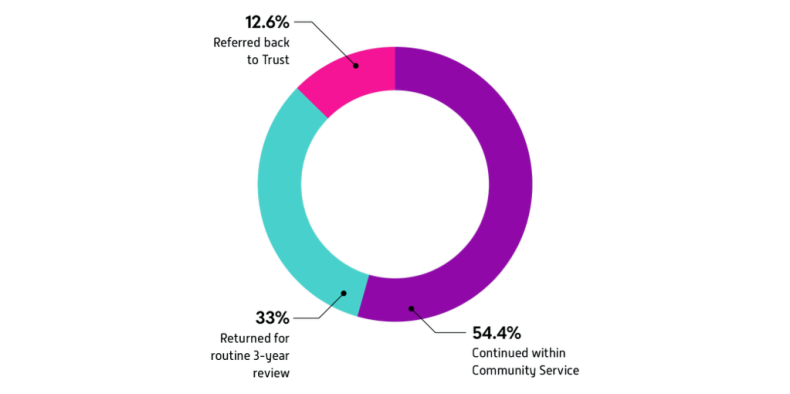
Between 2021 and 2025, the service has supported more than 3,300 patients demonstrating both sustained demand and strong capacity within the community glaucoma monitoring model. Of these, 12.6% were red flagged and referred back to trust care, ensuring timely specialist intervention for those with higher risk or changing clinical needs. A further 33% were returned for routine three-year reviews, supporting ongoing surveillance and continuity of care. The remaining 54.4% continued to be managed within the community service, reflecting its effectiveness in providing stable, long-term monitoring.
Greater Manchester
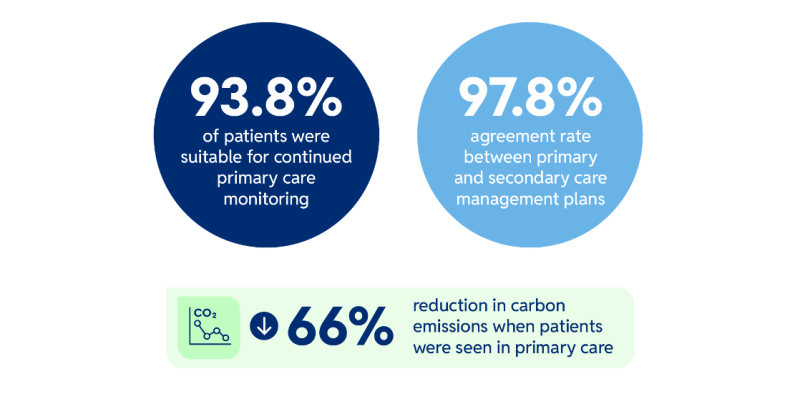
The Primary Eyecare Glaucoma Service (PEGS) pilot ran for three years and concluded around mid-2025. The evaluation, co-authored by Manchester Royal Eye Hospital and Primary Eyecare Services, demonstrated 93.8% of patients were suitable for continued primary care monitoring, there was a 97.8% agreement rate between primary and secondary care management plans. In addition, carbon emissions were reduced by approximately two-thirds when patients were seen in primary care.
Further information
For more detail on this improvement insight, contact Primary Eyecare Services.
Also take a look at our new programme to support teams to understand, plan and create the infrastructure and processes needed to move ophthalmology services into the community.



