Unlocking the potential of primary care provider collaboratives
Primary care provider collaboratives are fundamental to the successful delivery of a neighbourhood health service. Their role will be pivotal in shifting care from hospitals to community, reducing health inequalities and ensuring that everyone has access to high-quality care.
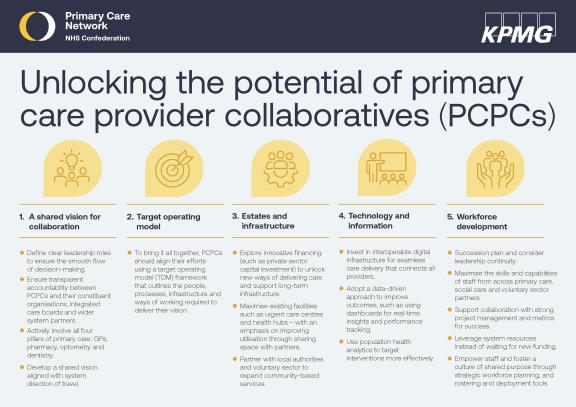
In partnership with KPMG, the NHS Confederation's Primary Care Network has been exploring what is needed to unlock collaboratives' potential. This infographic captures five key aspects:
- A shared vision for collaboration
- Target operating model
- Estates and infrastructure
- Technology and information
- Workforce development



