Primary care recovery plan: what primary care leaders need to see
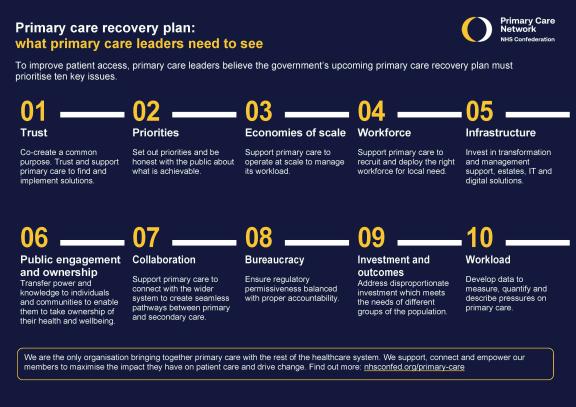
Trust
Co-create a common purpose. Trust and support primary care to find and implement solutions.
Priorities
Set out priorities and be honest with the public about what is achievable.
Economies of scale
Support primary care to operate at scale to manage its workload.
Workforce
Support primary care to recruit and deploy the right workforce for local need.
Infrastructure
Invest in transformation and management support, estates, IT and digital solutions.
Public engagement and ownership
Transfer power and knowledge to individuals and communities to enable them to take ownership of their health and wellbeing.

Collaboration
Support primary care to connect with the wider system to create seamless pathways between primary and secondary care.
Bureaucracy
Ensure regulatory permissiveness balanced with proper accountability.
Investment and outcomes
Address disproportionate investment which meets the needs of different groups of the population.
Workload
Develop data to measure, quantify and describe pressures on primary care.
About the Primary Care Network
We are the only organisation bringing together primary care with the rest of the healthcare system. We support, connect and empower our members to maximise the impact they have on patient care and drive change. Find out more.



