What is population health?
This explainer provides an overview of population health and the strategic approach taken in Wales. It explores the key factors that influence health, often referred to as the wider determinants of health, and examines the current health challenges facing the Welsh population. The explainer also discusses the strategic framework and legislation that guide NHS Wales's efforts to create a healthier, more equitable future, highlighting both the opportunities and the emerging challenges that lie ahead.
What is population health?
According to The King’s Fund’s definition, population health is an approach focused on improving the health of an entire population. It is about enhancing the overall physical and mental wellbeing of people within a specific community, region or nation, while also reducing health inequalities.
This involves preventing illness, providing effective health and care services, and addressing the broader factors that influence health, all in collaboration with communities and partner organisations. These efforts are often led by or involve public health specialists and teams. Further information about public health teams can be found in our explainer, What is public health?
What is population health management?
Population health management is a data-driven approach that combines health information to identify specific groups within a population. Health and care systems can then prioritise these groups for tailored support and services. For instance, data might be used to identify frequent users of emergency departments, allowing for targeted preventative actions to improve their health and lessen the strain on acute services.
What factors are considered as part of population health?
Population health looks beyond the individual patient and considers a broad range of factors, known as the "wider determinants of health", that influence wellbeing. These factors can be classified into several key areas:
- Social, economic and cultural (social determinants of health): These are often considered the most significant drivers of health. They include income, education, employment, social support networks, housing (including living conditions), food security (and access to healthy food) and experiences with discrimination, racism and violence.
- Physical environment and ecosystems: This refers to the natural and built environments where people live, work and play. They include air and water quality, safety of neighbourhoods and transportation systems, access to green areas, biodiversity, climate and exposure to pollutants and environmental hazards.
- Individual behaviours and lifestyle: These are individual choices and habits that affect health, such as diet and nutrition, physical activity levels, tobacco and alcohol use and reacting to stress.
- Healthcare access and quality: This remains an important determinant of health. It includes access to healthcare services and social care, quality of care, including preventative services and treatment and the effectiveness of public health interventions.
- Individual biology: An individual's biology also plays a significant role in their health. This includes their age, sex and genetic predisposition to certain diseases and conditions.
What are the key population health challenges in Wales?
There are a number of significant health challenges facing the Welsh population. For example, the leading causes of death in Wales in 2023 were:
- Dementia and Alzheimer’s disease: 10.6%
- Ischaemic heart diseases: 10.4%
- Chronic lower respiratory diseases: 5.9%
- Malignant neoplasm of the trachea, bronchus, and lung: 5.1%
- Cerebrovascular diseases: 5.0%
- Influenza and pneumonia: 4.3%.
Mental health:
- In 2024 to 2025, 33% of adults reported low mental wellbeing, 52% medium and 15% high. Lower scores were linked to deprivation, younger age, poor physical health and loneliness.
Healthy behaviours:
- Healthy lifestyle behaviours: Only 93.6% of adults reported engaging in two or more of five healthy lifestyle behaviours (fruit and vegetable consumption, not smoking, drinking within guidelines, being physically active, healthy weight) in 2024 to 2025.
- Overweight and obesity: Approximately 60% of adults in Wales are overweight or obese, following significant increases in the last few decades.
- Smoking prevalence: Smoking prevalence has now declined to 12.6% as of 2023.
- Drug and alcohol-related avoidable mortality (Drug and Alcohol-related): This continues to rise steadily, from 24.2 per 100,000 population in 2019 to a record 30.2 per 100,000 in 2022.
What is the current strategic approach to population health?
A Healthier Wales is the Welsh Government's long-term plan for health and social care, aiming to improve population health and wellbeing. Key to this is a focus on prevention, early intervention and addressing health inequalities. The plan emphasises shifting services towards primary care and community-based, holistic provision.
The latest NHS Wales Performance framework includes several performance measures under prevention relating to population health. In addition, Wales has a number of enabling policies and duties for improving population health and wellbeing and reducing health inequalities, as set out below.
What are the emerging challenges and opportunities for population health in Wales?
Challenges
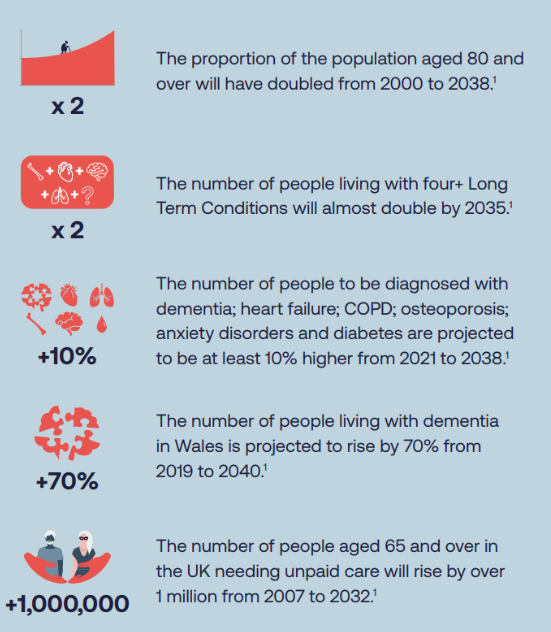
The Future Trends Report Wales 2021 set out several key drivers and trends facing public bodies in Wales, including the NHS, that present both challenges and opportunities. See page 2 of this infographic document in particular.
Here's a snapshot of some of the projected population health challenges in Wales:
Opportunities
The Well-being of Future Generations Act sets out the five ways of working for public bodies to help them sustainably meet and improve the wellbeing of their populations in a way which will protect future generations too:
- Long-term thinking: Balancing short-term needs with the needs to safeguard the ability to also meet future needs
- Prevention: Acting to stop problems occurring or getting worse
- Integration: Considering how our objectives impact on the well-being goals and other objectives
- Collaboration: Working with other parts of the organisation and other bodies
- Involvement: Involving people with an interest in achieving the well-being goals and ensuring those people reflect the diversity of those we affect.
Public Health Wales has also worked with the Office of the Future Generations to produce several tools and methods for public bodies to think and plan for the future.
Finally, technology, including artificial intelligence, can potentially improve staff and patient wellbeing. For example, research and development by the NHS via Health and Care Research Wales or the work of the Welsh life sciences sector. The Welsh Government’s digital and data strategy for health and social care in Wales sets out keys aims and actions, such as the development of the NHS Wales App and roll-out of electronic health records and prescribing, building on the creation of Digital Health and Care Wales. However, as technology is developed and implemented, it is vital that there is meaningful staff and patient engagement that accounts for diversity and addresses issues such as digital exclusion. Otherwise, new health technologies can risk potentially exacerbating existing health inequalities.
Summary
Improving the health of the Welsh population is a complex task that extends far beyond traditional healthcare settings. The data shows that while some progress is being made in areas like healthy behaviours and smoking prevalence, significant challenges remain, particularly in areas such as obesity, mental wellbeing and drug and alcohol use. However, by leveraging key strategic policies and legislation, such as A Healthier Wales and the Well-being of Future Generations Act, NHS Wales is working to address these issues holistically. The focus on prevention, collaboration, and a long-term approach will be critical in tackling health inequalities and ensuring a healthier and more equal Wales for generations to come.



