Exploring adult social care funding and delayed discharge
Key points
- This briefing sets out what funding the government has recently announced and how this is being put to good use.
- In November 2022, the Autumn Statement announced new funding for adult social care of up to £2.8 billion in 2023/24 and up to £4.7 billion in 2024/25.
- This funding comes after a decade of falling local authority budgets and what’s been announced remains far short of what’s needed to alleviate pressure on local authorities and the NHS.
- The Local Government Association has called for £13 billion to meet this combination of ongoing pressures and to ensure councils can meet all of their statutory duties under the Care Act.

Overview
This briefing sets out detail and commentary on the funding announced for adult social care in the 2022 Autumn Statement. It does so in the important context of delayed discharge, offering joint Local Government Association and NHS Confederation illustrative thinking on the kind of actions that could be taken to help address immediate pressures in hospitals.
What new funding has been made available for adult social care overall?
In November 2022, the Autumn Statement announced new funding for adult social care of up to £2.8 billion in 2023/24 and up to £4.7 billion in 2024/25. Our understanding is that the funding breaks down as follows:
|
Funding source |
2023/24 £m | 2024/25 £m | Notes |
|---|---|---|---|
| Social care grant | 1,265 | 1,877 | Repurposed funding from the delay to adult social care charging reform and for both adult and children’s social care. |
| New grant | 400 | 683 | Ring-fenced for adult social care and which will also help to support capacity and discharge. In 2023/24, the £400 million will be combined with £162 million of continued Fair Cost of Care funding, totalling £562 million in 2023/24. |
| 600 | 1,000 | Distributed through Better Care Fund to help get people out of hospital. | |
| New council tax flexibilities | 550 | 1,170 | For 2023/24 and 2024/25, councils can increase both council tax and the adult social care precept by 1 per cent each to 3 per cent and 2 per cent respectively. The stated figures assume councils will raise the maximum precept and council tax and that the additional funding from the increase in council tax will go to adult social care. |
| Total (rounded) | 2,800 | 4,700 |
What impact will this funding have?
The government has described the funding announced in the Autumn Statement as record investment that will “put the adult social care system in England on a stronger financial footing and improve the quality of and access to care for many of the most vulnerable in our society”.
However, the funding needs to be considered in the context of both what councils will potentially receive and the scale of pressures on adult social care they face.
What new adult social care funding will councils receive?
It is difficult to predict how much new funding for adult social care councils will receive over the next two years. However, it is unlikely that they will receive the full £2.8 billion (2023/24) and £4.7 billion (2024/25) that the government continues to refer to. Key underlying factors are:
- The headline figures announced in the Autumn Statement relate to funding for adult social care as a whole, rather than funding that would necessarily be available to councils. Specifically, the funding for the adult social care discharge grant will be split between councils and health bodies. Consequently, councils will receive £800 million over the next two years from this grant rather than the full £1.6 billion.
- For each of the next two years, social care councils are able to raise their council tax rates by up to 3 per cent without requiring a referendum. They can also raise an adult social precept of up to 2 per cent. Both of these thresholds are one percentage point higher than 2022/23. The headline adult social care figures announced at the Autumn Statement assume that all social care councils will raise both their council tax and adult social care precept to the maximum. The headline figures also appear to assume that councils will allocate all the additional income raised from the increase in the council tax rate threshold, to adult social care. Consequently, the assumed new funding from council tax flexibilities is best seen as a potential maximum amount, rather than as guaranteed new income to support adult social care.
- The social care grant provided to councils will increase by £1.265 million in 2023/24. However, this grant is not prescribed solely for adult social care and can also be used for children’s social care. The Association of Directors of Adult Social Care Services’ (ADASS) 2022 survey indicates that, on average, councils allocated 41 per cent of their 2022/23 allocation of this grant to children’s social care.
In addition to the specific issues about council tax above, it must be noted that there is a mismatch between council tax as a funding source for adult social care and the amounts that can be raised through small percentage increases in the adult social care precept, particularly in areas of highest need.
How does new funding compare to councils’ cost and demand pressures?
Councils’ adult social care budgets are a moving target. Patterns of spend do not stand still from year to year. Instead, inflation, wage pressures and demographic changes constantly erode available resources. Councils seek to address these issues by making annual savings within their overall adult social care budgets. Nonetheless, because of the constant pressure on the core elements of councils’ adult social care budgets, when councils do receive new funding, it is not necessarily all available to support entirely new service provision or to address new forms of demand. Rather, despite councils’ annual savings and efficiencies programmes, in many cases a proportion of new funding is needed to help address the unrelenting demand and cost pressures faced councils’ existing adult social care services.
At the current time, councils face a range of cost and demand pressures, including:
- a 9.7 per cent increase in the National Minimum Living Wage in 2023/24
- a forecast 5.5 per cent increase in CPI inflation in 2023/24, following on from 10.1 per cent in 2022/23
- demographic pressures of £686 million in 2022/23, according to the 2022 ADASS survey.
Given these pressures, and the points above that not all of the announced funding may actually be raised (council tax/precept) or go to adult social care (some will go to children’s social care), it is highly unlikely that that the investment will do anything other than enable adult social care to stand still. It is therefore essential that government and/or systems do not raise expectations unfairly; the funding provided will not all be used to enable significant additional capacity or action on other key issues, such as care worker pay.
These deep-seated issues need to be addressed to put adult social care on a long-term, sustainable footing. Overall, the Local Government Association has called for £13 billion to meet this combination of ongoing pressures and to ensure councils can meet all of their statutory duties under the Care Act. This includes £3 billion towards tackling significant recruitment and retention problems by increasing care worker pay. An investment of this scale is needed to support our national infrastructure, our economy and our prosperity. People who draw on social care and support will remain concerned about the services they access to live the lives they want to lead.
Will the money get through to adult social care or could it be spent elsewhere?
Councils have faced significant financial challenges in recent years, including the loss of £15 billion in government funding from 2010/11 to 2019/20. Throughout this period, councils have sought to protect spending on adult social care. Children’s social care spending has also been protected. As a consequence, it has predominantly been councils’ non-social care services that have faced significant reductions in council spend.
Figure 1: Change in English councils’ budgeted net spend by service area, 2010/11 to 2022/23
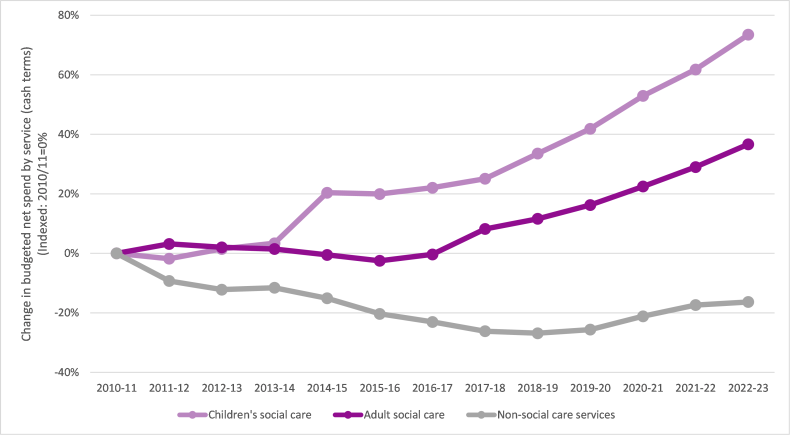
Source: Local Government Association analysis of revenue account budget data published by the Department for Levelling Up, Housing and Communities (DLUHC).
- In 2014/15 there was a definitional change in the data for children's social care (which increased spend by c£1 billion). The data is comparable from 2014/15 to 2022/23.
- Non-social care services include planning and development, central services, environmental services, housing services (non-HRA), culture and leisure, and transport and highways.
- We exclude local authority spending on education services, public health and ‘other services’. Public health only became a council responsibility in 2013/14.
- Housing services spend is general fund revenue account expenditure and excludes the housing revenue account.
- We show data for London borough councils (including the City of London) metropolitan district councils, shire county councils, shire district councils, and unitary authorities.
- Data shown is budgeted net revenue expenditure. This is spending funded by councils’ own resources such as council tax and business rates, and also from government grants. NHS transfers to adult social care are not shown in this chart as they are not included in the budget data published by DLUHC. For the same reason, spending supported by sales, fees and charges income is also not included.
It is also crucial to bear in mind that the non-social care services that have faced a disproportionate reduction in funding to protect social care services include those that contribute to wellbeing and prevention in their widest sense. Services such as housing, leisure, transport, parks and green spaces, and skills – as well as funding to local voluntary and community sector initiatives – all play an important role in the ecology of local communities, supporting people to be well and tackling the wider determinants of ill health.
What new funding has been made available to specifically target delayed discharge?
Adult Social Care Discharge Fund
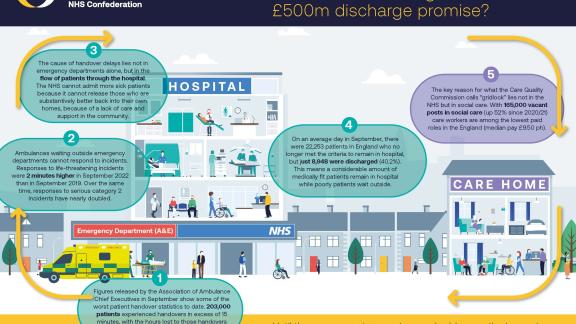
In September 2022, the government’s Plan for Patients announced £500 million to help get people out of hospital and into social care support. It was described as a first step that will inform “further action from next year to rebalance funding across health and care, to establish a strong and sustainable social care sector with greater accountability for use of taxpayers’ money.” Further information in November 2022 confirmed that:
- £200 million will be distributed to local authorities
- £300 million will be distributed to integrated care boards (ICBs), targeted at those areas experiencing the greatest discharge delays
- there is an expectation that the funding will be pooled into the Better Care Fund
- the funding will be provided in two tranches: 40 per cent in December 2022; 60 per cent by the end of January 2023
Speeding up discharge
In January 2023, the government announced £250 million to further speed up hospital discharge. The bulk of this funding, £200 million, will be used by ICBs to fund maximum stays of up to four weeks per person in care homes and other settings with wrap around support by the end of March. The balance, £50 million, will be capital funding to upgrade and expand hospitals.
What is the best way to spend the £500 million for maximum impact?
We believe the following kinds of short-term actions could be taken now to help address immediate pressures in hospitals, as well as medium-term actions that will help preparations for next winter. These are illustrative and intended to help shift the focus away from thinking that simply buying more care home beds is the solution to the challenge of delayed discharge.
Short term
- Focus on simple discharge: make sure people without complex needs are discharged rapidly.
- Invest in voluntary sector support: this can mobilise quickly and provide access to an additional workforce. Services such as ‘sitting services’ (which provides reassurance for people who may not need care but are concerned at being alone after discharge), unpaid carer support, handyperson services, and home-from-hospital services can all play a key role in meeting low-level needs after discharge, as well contributing to preventing possible readmission.
- Invest in therapeutic-led reablement: intensive short-term interventions with follow-up support can support recovery after time spent in hospital.
- Increase care worker pay: pay, including one-off increases and/or retention bonuses, can help tackle the serious recruitment and retention issues facing the sector.
- Invest in alternatives to home care, such as:
- one-off discharge personal budgets to buy anything that would aid recovery or could be backfill pay for a family member taking time off
- discharge personal assistants with a small budget to help person settle and/or arrange longer-term support
- bursary to attract 18-25 year olds to care work
- ‘telecare in a bag’ kit (this is the issuing of care technology to people directly from hospital. This might be, for example, a handset with an emergency button which can be linked to an emergency monitoring centre. This solution ensures that people can get home quickly but with support in place should it be needed).
Medium term
- Focus on prevention and recovery services, including steps to support the voluntary sector to provide fast, low-level support is essential.
- Build on the good work being done in some areas to identify and target the people most at risk of admission.
- Invest properly in primary and community services.
- Tackle the long-standing issue of care worker pay.
What are some examples of innovation and best practice on delayed discharge?
National Discharge Frontrunner sites: Humber and North Yorkshire Health and Care Partnership
In June 2022, NHS England sought expressions of interest from local systems to lead the way in developing and testing radical new approaches to discharging people from acute care. After a competitive selection process, over a number of months, Humber and North Yorkshire Health and Care Partnership has now been selected as one of six sites selected nationally as a Discharge Frontrunner.
The main objective of the Humber and North Yorkshire programme is to ensure more people are supported to leave acute care and have the right support, in the right place, in a safe and timely manner. Technology is at the heart of this to enable a ‘single version of the truth’ – this will highlight any delayed discharge, who owns the delay, and provide alternative pathway capacity to help expedite to alternative community provision.
The technology being implemented is an application built in collaboration between NHS, social care and voluntary, community and social enterprise organisations. This is called Community OPTICA and tracks the total community capacity across the health and care system for the purpose of admission avoidance and timely discharge.
The successful Discharge Frontrunner sites were announced in January 2023, and the Humber and North Yorkshire scheme will now begin implementation using a phased programme over the coming months, looking to integrate further partners as it does so. The scheme will run for 12 months as a pilot, but it is hoped that this can be extended beyond the initial period and replicated across the country.
About Humber and North Yorkshire Health and Care Partnership
Humber and North Yorkshire Health and Care Partnership is one of 42 integrated care systems (ICSs) which cover England to meet health and care needs across an area, coordinate services and plan in a way that improves population health and reduces inequalities between different groups. The partnership comprises of NHS organisations, local councils, health and care providers and voluntary, community and social enterprise (VCSE) organisations.
Working across a large geographical area, Humber and North Yorkshire includes a population of 1.7 million people and incorporates the cities of Hull and York and the large rural areas across East Yorkshire, North Yorkshire and Northern Lincolnshire.
Intensive implementation of D2A Home First: North Cumbria
Background
The LGA was approached in June 2020 by North Cumbria to carry out a peer review. Cumbria had received several interventions over recent years to help address performance issues in relation to flow, particularly hospital discharge. While some improvements were achieved in the short term, these had not been sustained. Through the Better Care Support Team (BCFT) bespoke support programme run by the LGA, a team of peers was convened to act as a critical friend and support improvement.
Making the change happen
- Recognised that it needed support to break the cycle and make change happen.
- LGA/Emergency Care Improvement Support Team (ECIST) executive enquiry – short, focussed; quickly identified strengths, opportunities for improvement, and an action plan
- Brought system's executives together weekly in focused way – forged strong system leadership (regular input from LGA/ECIST)
- Fortnightly Health and Social Care Group – led by LGA/ECIST colleagues – sharing learning, building relationships, breaking down historical barriers and narratives in a safe space (shared understanding and effective leadership at all levels).
- Recruitment of home first system coordinator – impact of this post, holding all parts of the system to account has been really powerful. The team do not think they would be where they are now we it not for the role in terms of challenge, holding the mirror up and delivering change at pace.
Tools to support change
- Welcomed the challenge into the system – the push back against the blame culture – and realisation that delays in the system were not down to one partner.
- Ongoing support, knowledge, experience and networking opportunities that working with the LGA and ECIST has brought has been invaluable.
- Dedicated workshops to help understand and better define offer and impact for seven-day transfer of care hub.
- Commissioning, home-first models, assistive technology – learning from others, together.
- Flexibility of in-house provider and relationships with independent sector.
Outcome
- Improved flow through hospitals.
- Huge reduction long length of stays.
- Improved ambulance handovers.
- Improved discharge experience for patients and providers.
- Streamlined effective information gathering prior to discharge and agreed with providers.
- Improved daily reporting that informs areas for focused attention.
- Improved morale and motivation.
- Co-production and the opportunity to influence change.
- Greater understanding of each other’s roles, responsibilities and realities.
- Celebrating as a system is really powerful and shared ownership of the risks and challenges that we face everyday.
Hospital discharge: Stockton-on-Tees Borough Council
‘I don’t have many friends and family, the help the staff gave me put my mind at ease, I’m not sure what I would have done without them. I was very worried about how I would manage at home after being unwell, but the support was there the same day I got home and was very good.’
This is George’s experience of the partnership between Stockton-on-Tees Borough Council, North East and North Cumbria Integrated Care Board (ICB) and North Tees and Hartlepool NHS Foundation Trust, which operates a collaborative, integrated and embedded model of care for hospital discharge. Organisational commitment and the positive relationships between staff from each organisation have resulted in the creation of joint strategic planning and joint operational decision making that focuses on achieving good outcomes for people leaving hospital.
Professional opinions across health and social care are equally valued and forward planning and early, effective communication are key to the hospital discharge model. Daily multi-disciplinary huddles and weekly strategic planning meetings take place to ensure there is a ‘no surprises’ approach. Hospital discharge services can be time sensitive, and this can lead to a high-pressured environment, however these challenges have been overcome with effective continuous communication and engagement enabling multiple professionals from a variety of organisations to pull together for the same goal, providing personalised support to people.
A critical element of the model is forward planning with commissioning, finance, and procurement teams. Intelligence collated by partners is used to develop and support the delivery of appropriate responsive and flexible services with our independent care provider market.
The local system wrapped around North Tees and Hartlepool NHS Foundation Trust is enabling timely and effective hospital discharge, supporting people to move to an environment they can thrive in. The performance indicators of criteria to reside and length of hospital stay (7+, 14+ and 21+ days in hospital) all show that the local system performs as one of the best across all indicators.
What should we learn from this ahead of next winter?
Local authority and healthcare leaders welcome the additional discharge funding on top of the Adult Social Care Discharge Fund the government announced last September. However, the last-minute and short-term nature of the funding does not match the more fundamental challenges the health and care sector is facing – the widening gap between the capacity, resource and need.
In addition, short term, prescriptive funding pots limit the ability of the sector to innovate, creating more risk that we invest into extending existing services rather than reimagining more joined-up care that makes best use of staff available.
Discharging more patients from hospital into care homes will help flow and is a better alternative than medically fit patients being prevented from leaving hospital. However, it also runs the risk of people being inappropriately placed and remaining in residential provision indefinitely. The risk of this is heightened by needing to make rapid decisions around care and arrange full wrap-around support required for people to make full recoveries. The implementation of the interventions is further hampered by the substantial reporting burden attached to the funding – the specificity of criteria and volume is significantly constraining flexibility and adding bureaucratic pressure.
Next winter, the government must set out its plan for winter well in advance of the season, so that systems can design and deliver solutions that are appropriate to the local challenges they face. These will be more sustainable, make the best use of limited resource and work towards the best outcomes for all patients. This includes the government setting out and sticking to a clear timetable for when funding reaches the frontline, allowing flexibility in how it is spent, and reviewing the reporting requirements. This must also provide clarity around future funding availability so interventions can become lasting solutions.
Strengthening community capacity in both health and social care is the answer but this takes investment and time. Unless record low staffing levels and low pay are addressed it will be nothing more than a winter quick fix, and the same problems will return.