Working in systems: a practical guide for clinical and care professionals

Introduction
Between August 2022 and April 2023, the NHS Confederation brought together a clinical and care professional leadership learning network, which included a broad cohort of clinicians, care professionals and appropriate non-clinical staff outside of formal leadership positions across the health and care sector.
Its aim was to engage in the principles and ideas related to clinical and care professional leadership, as set out in national guidance, and to empower professionals to think differently about their roles within the systems that they operate, not just their organisations.
Increased collaboration of clinical and care professionals across organisations should offer patients and service users an improved experience of health and care services; and the evidence suggests that strong leadership leads to better health outcomes. 1 2 3
The group has developed this practical guide to support other professionals across the country to engage in these principles and to become leaders in collaboration themselves. The guide includes:
- top tips for collaboration
- lessons learned
- go-to resources that have helped them on their leadership journeys.
Top tips for collaboration
Top Tip #1
Invest in your relationships with your partners
Members put forward several tips to improve partnership working, but one consistent theme was that taking the time to build relationships is essential. This means not just valuing relationships in everything that you do but explicitly setting aside time to invest in them despite the time pressures you face.
Having relationships with key people of influence and decision-makers in each organisation will help mobilise activity and encourage progress. This can be facilitated by spending time with partners to get to know them as individuals.
Members emphasised the importance of striving to understand the perspective of your partners and pursuing win-win outcomes, not takeovers.
Top Tip #2
Outline a clear purpose and define roles and responsibilities
Members highlighted the importance of setting a clear and common goal with partners, building on the relationships that have been established and acknowledging shared challenges. Agreeing on the purpose of the project or programme is key. Focusing on the ‘why’ and asking difficult questions can help you stay on track.
Members shared that no meeting should ever be left begging the questions: “What did we agree?” or “Why are we doing this?”
Alongside clarity of purpose, expectations of each partner should be set out as early as possible. Everyone should have a clear understanding of how their role contributes to the aims of the project or programme – this helps ensure buy-in from staff at all levels to make it successful.
Top Tip #3
Be empathetic and flexible to build trust
There are many ways that partnership working can be improved. Striving to understand the needs and pressures of your partners can help you work to solutions that work for everyone. A win-win is great if you can achieve it, but sometimes partners must be flexible to meet aims and, for you as an individual, demonstrating flexibility to your partners shows your commitment to genuine collaboration.
A crucial part of flexibility is being clear on areas to negotiate on and what your red lines are.
Managing conflict can be challenging and you must be prepared to deal with divergent views. In their experience, members highlighted that negative feedback shouldn’t be disregarded but used positively, as a catalyst for change and growth.
Following through on actions and taking an inclusive approach will help you earn the trust of your partners. This should include seeking the views of quiet or silent participants in meetings or on a one-to-one basis.
Top Tip #4
Give people the space to invest in system thinking
Releasing time and giving permission for leaders across the integrated care system to come together to understand system working and contribute to decision-making is vital. System thinking becomes the norm by having a leadership model at place and throughout the system that people can buy into when given the space.
On an individual level, protecting some time for yourself each week for strategic thinking and planning makes it easier to work effectively.
Top Tip #5
Build research and evidence into all decision-making
To make effective, collaborative decisions, members suggested that clinical and care professionals should use research and evidence to inform their decision-making, ranging from clinical research evidence to data on patient experience. Being data-led reduces the influence of biases and helps to ensure all partners are pursuing the right common goal.
To help improve outcomes for our populations, encouraging and facilitating colleagues to get involved in research and promote research opportunities to patients and service users is essential.
That does not always mean, however, that you must only focus on data. Visiting services and talking to clinicians, patients and the public to hear their perspectives is at the heart of this work. Clinical and care professional leadership within systems means working with people and communities.
Case study: The role of primary care leaders in integrated care systems
In February 2023, South East London Integrated Care System (ICS) held a clinical and care professional leadership session to discuss:
the involvement of primary care leaders in the work of the ICS the leadership needs of those involved how the ICS can play a role in supporting their development.
I was invited to chair the session, which convened 25 leaders from the six PCNs in the London Borough of Lewisham, including from general practice, super-practices, local medical committee representatives and the chief executive of the GP federation.
“...clinical leaders did not need more knowledge or training to support their development – they needed time and space."
Purpose
One of the key purposes of the session was to try and work towards a unified primary care voice for Lewisham.
Results
The session led to two outcomes:
- The terms of reference to help manage the group going forward.
- It was agreed that the chair was not only to be paid but also objective/impartial, which the group felt was really important.
Conclusion
I found that, as suggested by the NHS England guidance on clinical and care professional leadership, providing these leaders with the space and time to have this discussion was really fruitful. Setting ground rules early enabled free-flowing and honest conversations.
It was a mature environment for clinical leaders to have difficult conversations and see each others’ points of view.
What was clear to me more than anything was that clinical leaders did not need more knowledge or training to support their development – they needed time and space.
Tara Humphrey, Network Manager, Warrington Innovation Network and Primary Care Network (PCN) specialist
Case study: Creating a culture of shared learning, collaboration and innovation
The Clinical Research Network Greater Manchester (CRN GM), a network of the National Institute for Health and Care Research (NIHR), and Greater Manchester Integrated Care System (GM ICS) have been creating a culture of shared learning, collaboration and innovation, through several joint ventures.
Sarah Fallon, chief operating officer at the CRN GM and Warren Heppolette, chief officer for strategy and innovation at GM ICS share examples of this collaboration.
Example 1: Greater Manchester NIHR oversight board
The oversight board brings together the Applied Research Collaboration (ARC), Biomedical Research Centre, Clinical Research Facility, Patient Safety Research Collaborative, Translation Manchester, Health Innovation Manchester, the Christabel Pankhurst Institute for Health Technology Research and Innovation and CRN GM.
Being part of this leadership group has offered leaders within CRN GM and GM ICS opportunities for co-creation and maximising resources across the local infrastructure for care development that is both relevant and inclusive to local people and provider partners. Most recently we have established an operational group to connect on programmes centering around equality, diversity and inclusion, workforce development and digital progression.
It has been incredibly rewarding working collaboratively to find solutions to align strategies across organisations, to increase the impact on the health and social care needs of our population and services.
Example 2: Integrated leadership and initiatives
We have aligned structures to integrate across multiple business and operational departments to combine efforts and compliment services and approaches across the local system. For example, we have included CRN GM representation on the GM ICS primary care board.
...through shared speciality leadership, we are able to raise awareness of research infrastructure support available...
Together, we are promoting research delivery across the regional social care and public health forums and shared specialty leaders to raise awareness of the infrastructure support available to enable more providers to get involved in offering research through local services.
Example 3: Working alongside local people and communities
The ICS CRN GM and ARC have successfully delivered the ‘Enhancing Effective Community Partnerships for Research in the Greater Manchester Integrated Care System’ project which was funded through NHS England’s REND initiative. This involves working across voluntary, community or social enterprise organisations and, specially for this programme, co-creating engagement strategies with the Caribbean and African Health Network.
Other programmes of work with the ICS include, Enabling Research in Care Homes (ENRICH), building tools such as the Ready for Research book for young people and accessible ways for local communities to share their views on regional research.
The CRN GM team will continue to support the ICS with research engagement across primary care, local authorities, care homes, community organisations, faith groups and local charities.
Sarah Fallon, Chief Operating Officer, Clinical Research Network Greater Manchester
Warren Heppolette, Chief Officer for Strategy and Innovation, Greater Manchester Integrated Care System
Lessons learned
Mistake #1
Not laying the groundwork for change
Members said that a common mistake they have made is to rush into solving a problem without properly understanding the issue or who needs to be engaged. This is particularly true with new teams, services and pathways. Lack of clarity in the aims and lack of involvement of teams involved early on makes it more difficult to get their buy-in later. Re-aligning the vision of the project is time consuming and unproductive – it should be avoided by ensuring clarity from the start. Quality improvement frameworks can also be used to correctly frame the problem and identify the right solutions.
Engaging a wide range of partners before delivery is also key and you shouldn’t underestimate how much time this process takes. This includes staff on the ground, who may not always get the opportunity to be involved in system working.
Mistake #2
Having too many priorities
A widespread mistake is to do too much, too soon. It is not possible to undertake many change initiatives simultaneously and attempting to do so can have leaders feeling overwhelmed. Setting a small number of priorities and delegating through a distributed leadership model will help you meet your goals.
Mistake #3
Not reaching out for help and avoiding difficult conversations
In moments of difficulty, members made the mistake of not asking for help or admitting when they got things wrong. Being honest when you do not know the answer and apologising for mistakes made is necessary to progress positively and to grow. Staying focused on the solutions can help you through these more challenging moments.
Partnerships can fail for a variety of reasons, and you may need to assess them at critical points. This may reveal, for example, that the project lacks resources or that trust has broken down between partners. Taking too long to have this difficult conversation may slow down progress. Listening to understand before addressing issues will help you navigate these challenging conversations.
Mistake #4
Making assumptions about partners and ways of working
Not everyone will understand or speak your own organisational language or match your culture. Members benefited from focusing on and highlighting their own biases which helped to support relationship management when circumstances change.
They added that it can be helpful to prepare to change your approach to keep stakeholders engaged and productive. It is not always possible to get full consensus between leadership teams, but an open mind and continued commitment to working collaboratively before key decisions can help you collectively navigate these challenges. From the experience of our members, a one-size-fits-all approach hardly ever works – flexibility is key. This is a fundamental trait held by system leaders, as opposed to traditional leaders.
Mistake #5
Keeping up a protectionist and individualistic behaviour
Maintaining a behaviour of protectionism and individualism is a common attitude that can undermine system working. Only thinking about yourself and your organisation is rarely successful and often encourages defensive behaviours from others. Unlearning a protectionist attitude implies clarifying what collaboration means and looks like at every step, particularly when it comes to budgets, accountability and commitment.
Members also highlighted that you should avoid trying to be directive towards partners – true collaboration means decisions are reached collectively, not at the discretion of vocal or forthright individuals.
Conclusion
Members hope that by putting into practice these tips and learning from their experiences, clinical and care professionals across the country can build on the great work they already do and work even more closely together – with the shared aim of improving outcomes for the communities they serve.
To learn more about this publication or the learning network, please contact:
Ian Perrin, Senior Policy Advisor – ICS Network, NHS Confederation at ian.perrin@nhsconfed.org
Skeena Williamson, Policy and Delivery Officer – ICS Network, NHS Confederation at skeena.williamson@nhsconfed.org
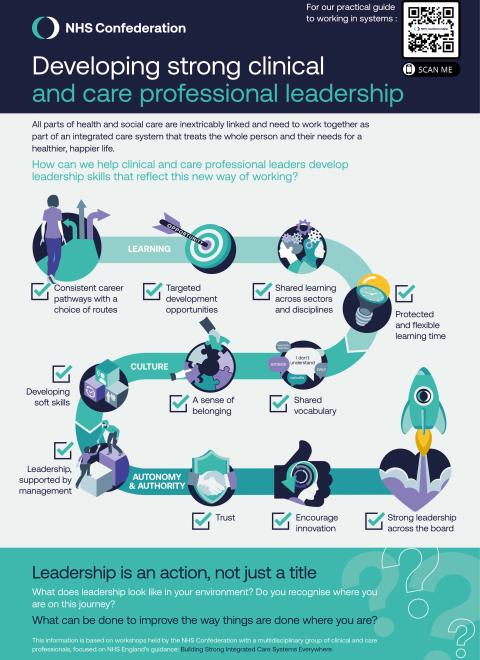
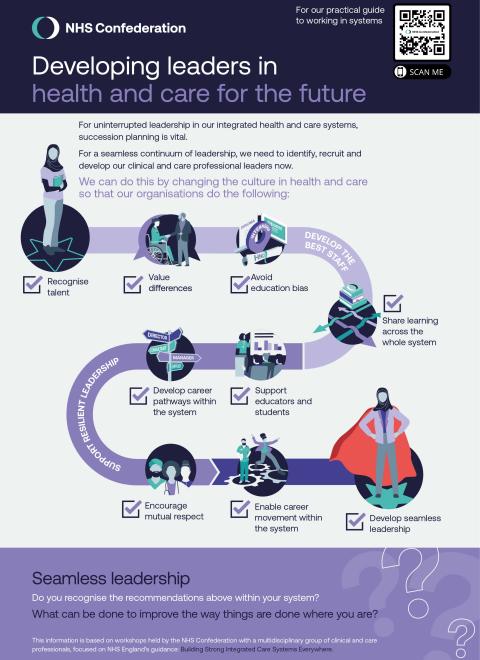
Leadership development resources
Acknowledgements
Footnotes
- 1. Prof West M., Dr Eckert R., Armit K., Dr Loewenthal L., West T and Lee A., Leadership in Health Care: A Summary of the Evidence Base. ↑
- 2. Guibert-Lacasa C., Vázquez-Calatayud M., Nurses' Clinical Leadership in the Hospital Setting: a systematic review, J Nurs Manag. 2022 May;30(4):913-925. doi: 10.1111/jonm.13570. Epub 2022 Mar 15. PMID: 35229386; PMCID: PMC9311216. ↑
- 3. Lyons O., George R., Galante JR., et al., Evidence-based Medical Leadership Development: a Systematic Review. BMJ Leader 2021;5:206-213. ↑