Does the NHS run 24/7?

The NHS currently faces an elective care backlog of over 7 million, and other parts of the system are experiencing backlogs too. While a backlog existed before the COVID-19 pandemic, it has climbed steeply as a result, with social distancing measures and the need for staff to be deployed to provide more urgent care playing a part.
As the service continues to make steady progress through the backlog – including making sure that virtually everyone who had been waiting two or more years for an elective treatment received one by the summer – some have been calling for the NHS to ramp up seven-day working.
The Secretary of State, Rt Hon Steve Barclay MP, has suggested that the backlog could be tackled more quickly if clinical staff worked more over the weekends. There have also been accusations aimed at primary care not providing sufficient weekend and evening appointments, and ongoing concerns about access to timely mental health support, especially for children and young people.
The Conservative Party’s 2015 manifesto promised a ‘seven-day NHS’, with the plan being to ensure patients could get the access they need to GP services, and for people in need of hospital care at weekends to receive the same high-quality care they would during the week. This was supposed to be achieved by 2020.
The background to this policy was a study that showed higher mortality rates among those who were admitted to hospital during weekends, suggesting that services then were insufficient. However, the findings have now been widely disputed.
So where did we get to with seven-day working? Is the Secretary of State right to imply it offers the key to tackling the backlog? What is happening already and what are the impediments to more of it? We explore these questions here.
Where did we get to with seven-day working?
Of course, many services have always run 24/7, such as ambulance services where staff work on a rota as is agreed in their contract, and for accident and emergencies such as serious injuries, heart attacks and strokes. General practice has always operated 24/7 care for urgent cases and the national 111 service has been in place since February 2014 (previously NHS Direct) for healthcare advice that does not require 999 support. Primary care networks (PCNs) are contracted to provide some general practice appointments on weekday evenings and Saturdays.
Members tell us that there is more evening, bank holiday and weekend working (referred to as out-of-hours working or OOH) than ever before in the NHS. A PCN with a patient population of 50,000 would tend to manage around 50 hours of ‘enhanced access’ appointments and calls a week. Pre and 'post' pandemic there has been expansion of OOH provision of outpatient, diagnostic and elective surgical lists, ramped up to address the elective backlog. Many trusts are known to get through many of their minor/low-risk procedures over weekends, including through locum support.
In 2013, to help ensure patients admitted in an emergency have access to the same high quality of inpatient care on every day of the week, NHS England (NHSE) developed the 7-Day Hospital Services (7DS) Programme. This introduced clinical standards, with NHSE requiring acute trusts to provide board assurance of compliance. There are good levels of compliance with these standards.
Many extra surgical and diagnostic lists are already being addressed at weekends compared to previously. This is partly due to the natural progression of the NHS offering more diagnostic and treatment options year on year as medicine advances and we treat older and more complex patients, for example with the availability of urgent CT scans over a weekend. Additionally, it is partly because of attempts to generate extra capacity to clear the elective backlog.
The below shows accident and emergency activity since 2020. It demonstrates that Monday is the busiest day and Saturday and Sunday the least busy, but with a relatively small margin:
So, in percentage terms the split of attendances show that in 2021/22 13 per cent of all attendances were on Saturday and 13.5 per cent were on Sunday (compared to 15.8 per cent at the highest for Monday).
Our members also tell us that they see lots of minor injuries during the weekend, from people being at home, perhaps doing DIY or children getting hurt playing.
As for other areas of the health service, community health services provide a wide range of services, with many operating out of hours, such as some palliative care services. All urgent community responses services are providing a rapid response service to people in their own homes 8am – 8pm, seven days a week. In some areas, such as North West London, that service has been extended until 10pm.
Similarly, health visiting services are often seven days a week, ensuring that mothers and young babies receive support within the first few weeks of a child’s life.
Some community health services provide an overnight community nursing service, providing urgent nursing care to housebound adults in their own homes, between the hours of 6pm to 8am, seven days a week.
Adult mental health crisis services often operate 24/7, and many areas have this for children too. Adult psychiatric liaison services, which work in acute hospitals, also operate 24/7. This is all in addition to the mental health crisis lines, which are often linked to NHS 111. These services are essential to providing the right type of support to individuals, particularly out of hours.
The NHS 111 Mental Health Triage Service is a good example of joint working between the mental health trust, the ambulance service and other partners to provide easy 24/7 access to support when people of any age, are experiencing mental crisis.
Impediments to seven-day working
1. Workforce shortages
The NHS is facing a workforce crisis with around 133,000 vacancies in England. In addition, primary care has lost more than 1,800 full time equivalent GPs since 2015. Members tell us that many NHS staff are feeling exhausted from a gruelling pandemic. There are simply insufficient staff to run services at full capacity (as they are run on a typical weekday) seven days a week. Some areas, such as maternity care, face especially acute shortages making these services particularly stretched.
Members of our Mental Health Network have said that in mental health, a shortage of consultant psychiatrists is an impediment to more out-of-hours working, as 1 in 10 posts are vacant. The men's psychiatric intensive care unit (PICU) in Lincolnshire has been closed temporarily due to staff shortages. These patients will likely be referred out of area, which the government has pledged to eliminate.
We must recognise that moving more staff to work out of hours reduces the number of staff available on weekdays as they are the same staff. NHS staff are also bound by the European Working Time Directive (unless they choose to voluntarily opt out), introducing minimum rules for employees relating to daily and weekly rest periods, rest breaks, annual leave entitlements, length of working week, and on night work. NHS staff are already largely at the contractual limit for hours worked, at 48 hours on average per working week, and due to workforce shortages are already picking up many extra shifts.
The government has agreed limits to junior doctors’ working hours and working patterns for reasons of safety: breaches of these are subject to fines set at four times the basic or enhanced rate of pay applicable at the time of the breach. The doctor will receive 1.5 times the applicable locum rate, the guardian will retain the remainder of the penalty amount.
In addition, more NHS provision requires more infrastructure. It is not just about more doctors, but more receptionists, cleaners and others integral to NHS provision and capital – buildings etc.
2. Pensions
For members of the NHS Pension Scheme, the value of pension savings is based on the growth in the member’s pension over the tax year. Pension growth is calculated by subtracting the value of the member’s pension at the start of the year (the opening value) from the value of the member’s pension at the end of the tax year (the closing value). If the member’s pension growth exceeds the annual allowance, excess benefits may be subject to a tax charge.
This is widely understood to be deterring doctors, including those working in primary care, from taking on extra hours as it may lead to tax penalties. NHS Employers, which is part of the NHS Confederation, wrote to the government calling for urgent changes to how NHS pension taxes are calculated. There was an indication that this issue would be addressed in the September 2022 fiscal event but detail has yet to materialise, and it was not included in October’s Autumn Statement.
Furthermore, not all providers of services outside of standard hours have access to the scheme. Sub-contractors of the PCN Enhanced Access service cannot offer the NHS Pension to staff they employ for that specific contract, reducing the appeal of working during the evening and Saturdays for them.
The government has launched a consultation on NHS pensions, which we hope will address some of the issues.
3. Cost
Although there may be potential savings from seven-day services through reducing lengths of stay in hospital, implementing the policy would add to overall hospital costs by 1.5–2 per cent as additional consultants would be needed to deliver these services.
There has always been considerable variation in NHS weekday and evening, weekend or bank holiday staffing provision. One reason for this is out-of-hours working is linked to weekend premium pay rates for many staff groups of additional pay between 30 and 94 per cent, depending on the pay band.
Therefore, the NHS gets more work for its money by prioritising using staff during their week-time contracted hours.
Out-of-hours working will also increase costs for estates and other infrastructure. Due to inflation and rising costs for things like energy, these bills are on the up. One Local Medical Committee recently proposed a reduction in core GP working hours to 9am-5pm, from the current 8am-6.30pm, to deal with the cost of running the premises.
In primary care, clinicians command a higher rate of pay for working the enhanced access service on weekday evenings and Saturdays, with one primary care provider supplementing rates by 20 per cent in the evening and 50 per cent on Saturdays. Additionally, opening the premises for longer hours also increases costs, including energy, which many primary care providers are struggling to meet. All of these costs must be covered by payments made to the PCN via the Network Contract DES, which has not been adjusted for inflation and it is unlikely payments will be increased to account for any uplifts to pay announced by the government, further eroding PCNs’ and GP practices’ finances.
Private sector working pays better than the NHS. So, if staff are going to work at the weekend, it will likely pay for them to do so in the private sector rather than the NHS, due often to higher rates of pay, and also due to the absence of the NHS penalties for working too many hours. If we start implementing measures that push staff away from the NHS into private sector, we will face even greater retention problems.
NHS guidance to trusts recognises the higher rate of pay for agency staff, and that they are often used to cover out-of-hours working.
Therefore, operating out of hours can cost more in salary payments through agency workers.
4. Staff morale and preference
Following the pandemic, NHS staff are experiencing unprecedented levels of exhaustion and low morale. This is exemplified by the finding of the annual NHS Staff Survey that staff morale fell between 2020 and 2021, and also by industrial action such as the recent vote by the RCN to strike, and the swathes of staff leaving the service, contributing to the 132,000 vacancies.
Alongside the gruelling pandemic that left staff feeling overworked, there have been ongoing disputes over pay, an issue that is being exacerbated by the cost-of-living crisis.
Asking staff to change to less sociable hours would deepen this sense of low morale and further disrupt the work-life balance for many. We would expect to see further NHS staff leaving the service – a loss that the NHS cannot bear.
The aforementioned Local Medical Committee suggestion that GP working hours are reduced to 9am-5pm was also supported by a number of others who feel the current working hours are ‘patriarchal’ and make working in the profession difficult for parents. This certainly suggests that further out-of-hours working is completely contrary to staff preferences and could serve as another push factor for staff to leave the NHS.
So, what can be done to help tackle the NHS elective backlog instead?
The NHS is already a 24/7 service, making sure patients get the care and support they need every day of the year. Access to and the range of services provided over evenings and weekends has increased over the years but a healthy dose of realism is needed about how able the NHS is to take on more non-urgent care over weekends with its current resources and the impact it would have on significantly reducing waiting lists. Significant increases in out-of-hours working alone is not a cost-effective or realistic solution to tackling the backlog. A number of other aspects need to be addressed first:
- The workforce plan promised in the recent Autumn Statement must be published as quickly as possible and must be fully costed and funded to ensure that the workforce projections it sets out can realistically be delivered. Health leaders are clear it must cover primary care too.
- The NHS Pension Scheme must be reviewed and adjusted so that doctors are not penalised if they choose to work more hours.
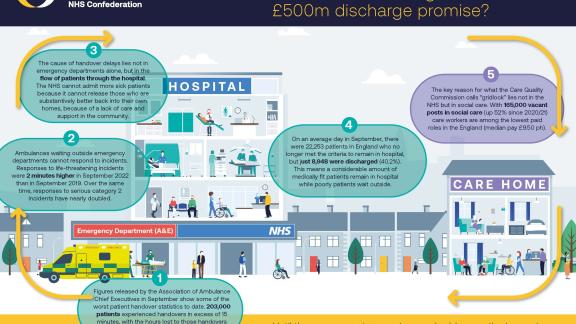
- Currently, due to a shortage of social care packages, the NHS is struggling to discharge medically fit patients into the community. For mental health, patients waiting for supportive housing is also delaying discharge. This is using beds that are needed by others and is exacerbating waiting times. The government confirmed a £500 billion Adult Social Care Discharge Fund to help with this in the Autumn Statement, alongside further funding announced for social care. However, health leaders have been reporting that it has come in too late to be used as effectively as it could have done had it been awarded earlier in the year. Also, the government needs to look at sustainable ways of recruiting and retaining staff in social care so that patients can be promptly moved into more appropriate care settings once they no longer need to be in hospital. One suggestion for this is to create a National Care Worker Minimum Wage of £10.50ph. The rise in the national living wage announced at the Autumn Statement was a good step towards this, but not to incentivise workers into social care over other jobs.
- Capital investment to address the £10.2 billion backlog in maintenance on NHS estate is important to improve efficiency in the NHS. In a recent survey, 9 out of 10 of our members told us their efforts to reduce the size of the waiting list are being hindered by a decade-long lack of investment in buildings and estate. This is also an issue primary care members face and is, likewise, particularly pronounced in mental health care.