2024/25 NHS priorities and operational planning guidance: what you need to know
Key points
On 27 March 2024, NHS England (NHSE) released its operational planning guidance for 2024/25, outlining the priority areas and objectives for the service.
We welcome recognition of progress and ambitions set out in the guidance. We also know leaders share NHSE’s determination to improve access to care and deliver more efficient services. There are concerns about how achievable the plans will be in the current context, but leaders are keen to build on the progress made in the last year.
Threats of further industrial action, including among general practitioners, long waiting lists and ongoing wider sector pressures, such as in social care, means 2024/25 is likely to be another tough year for all local services, their finances and ability to meet new stretching targets. For instance, increasing the performance target on four-hour waits to 78 per cent and requiring 95 per cent of diagnostic tests to be delivered within six weeks by March 2025, neither of which were achieved over the last year.
Despite this, the support organisations and systems will require to recover and make inroads against the targets listed, as well as locally defined priorities, is not clear. To give the NHS the best chance to recover, the government must end the industrial dispute that continues to impede progress on waiting lists, ensure system leaders have access to sufficient capital funding, increase investment in general practice and increase capacity in social care.
A central theme of the planning guidance is improving productivity. It confirms NHSE will report on productivity metrics at a national, ICB and trust level starting from the second half of the year. ICBs will also be asked to report on how well trusts are improving the primary–secondary care interface. NHSE should consider how to make these reporting processes as efficient as possible to maximise staff time.
While we support the focus on productivity and recovering A&E performance, there is a risk that focus is drawn away from some of the important actions outlined around increasing capacity in primary and community services and reducing health inequalities that will support the development of integrated pathways of care and improved health outcomes.
Looking ahead, given the clear impact of industrial action and uncertainties around the coming year, we recommend the objectives set out in this guidance are kept under review. In addition, that the government and NHSE aim to avoid publication of this guidance only days before its required implementation.

Overview
Priorities for 2024/25
NHSE’s overall aim in 2024/25 is around recovery of core services and productivity and asks systems to focus on the following priorities:
- Maintain collective focus on the overall quality and safety of services, particularly maternity and neonatal services, and reduce inequalities in line with the Core20PLUS5 approach.
- Improve ambulance response and A&E waiting times by supporting admissions avoidance and hospital discharge and maintaining the increased acute bed and ambulance service capacity that systems and providers committed to put in place for the final quarter of 2023/24..
- Reduce elective long waits and improve performance against the core cancer and diagnostic standards.
- Make it easier for people to access community and primary care services, particularly general practice and dentistry.
- Improve access to mental health services so that more people of all ages receive the treatment they need.
- Improve staff experience, retention and attendance.
Integrated care boards (ICBs), trusts and primary care providers are expected to work together to plan and deliver a balanced net system financial position in collaboration with other integrated care system (ICS) partners.
On recovery, NHSE refers systems to the already published plans for elective care; urgent and emergency care (UEC); NHS dentistry; and access to primary care, which set out essential actions. System plans are asked to reflect the needs of all age groups, including children and young people. The guidance promotes NHS IMPACT, NHSE’s new, single, shared NHS improvement approach to develop the leadership and organisational capacity, capability and infrastructure to create the conditions for improvement and deliver a small number of centrally led national programmes..
On the workforce, the need to improve bank management and reduce temporary staffing usage (especially off framework) is a priority. Alongside the key focus on staff experience and further improving retention, the guidance asks employers to consider implementing the new national pregnancy and baby loss people policy framework (with further guidance on menopause to follow). Work to improve the working lives of doctors in training (which is supported by NHS Employers, part of the NHS Confederation) is flagged. NHSE also reminds the NHS of the importance of its EDI transformation plan, published last year.
On improving productivity, NHSE expects ICBs and providers to work together to develop plans that deliver efficiency savings, raise productivity and implement more productive and flexible working practices, with a ‘relentless focus on improvement, reducing delays and unnecessary processes’. NHSE will report on productivity and supporting metrics at a national, ICB and trust level starting from the second half of 2024/25, with the intention to expand this to primary, community and mental health services. They will also work with systems on plans for the technology investment announced in the 2024 Spring Budget from 2025/26.
On transformation and planning for the future, the guidance proposes the following priorities:
- Expand evidenced-based approaches to prevention, self-care and the effective management of long-term conditions.
- Join up care closer to home through integrated neighbourhood teams and place-based arrangements.
- Integrate and streamline UEC pathways with a focus on the management of older people with complex needs and frailty.
- Continue to drive improvements in productivity and operational effectiveness.
- Work with higher education institutions and placement providers on key actions from the NHS Long Term Workforce Plan.
- Continue to support the levelling up of provider digital maturity, connect services to the NHS App, and engage with the national Federated Data Platform team.
National NHS objectives for 2024/25
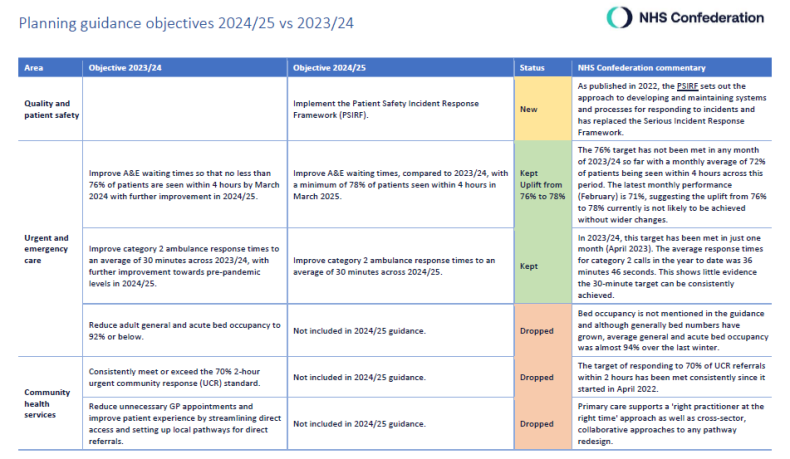
The guidance includes 32 objectives, covering 12 areas. View the priorities in the table below (click the + symbol to expand):
Click on the image below to access our table comparing 2024/24 objectives with 2023/24, including our commentary.
The following sections summarise NHSE’s key evidence-based actions to support delivery of the national objectives for 2024/25.
Quality and patient safety
Recover core services
Transform the way we deliver care and create stronger foundations for the future
NHSE plans to provide a progress update against the recovery plans, including an evaluation of the key actions. Further support is available on FutureNHS.
Planning assumptions and funding
NHSE has issued updated revenue allocations for 2024/25. ICBs will continue to receive Service Development Funding (SDF) allocations. For 2024/25 this will continue to be bundled into high-level groupings. Further detail is set out in the revenue finance and contracting guidance.
Core ICB capital allocations to 2024/25 remain the foundation of capital planning. Capital allocations will be topped up by £150 million nationally, in line with the incentive scheme for providers with a Type 1 A&E department. Further detail is set out in the capital guidance update 2024/25.
The contract default between ICBs and providers for most planned elective care will continue to be to pay unit prices for activity delivered. Activity targets will be agreed through planning as part of allocating ERF on a fair shares basis to systems.
Analysis
NHS leaders share the ambitions set out in the planning guidance and will do everything they can to improve access to care and deliver more efficiencies. However, they are receiving guidance on how to plan for 2024/25 just one working day before the start of the new financial year. This delay is unhelpful and points to a limiting short-termist approach from the government to long-term planning for the delivery of healthcare. Although this year has been particularly challenging due to industrial action, the government should work with NHSE to avoid such a delay in future.
We welcome the ambition to continue to develop services that shift activity to settings outside acute hospitals and into prevention and early intervention
We welcome the ambition to continue to develop services that shift activity to settings outside acute hospitals and into prevention and early intervention; one of our members’ top priorities for the next government. We also support the inclusion of the NHS IMPACT work to provide national leadership and create the conditions for improvement. Particularly important is its inclusion not only as a productivity and cost reduction driver but as a key support for quality and safety. The NHS Confederation fully supports this and plans to build on the ambition alongside NHSE with our support offer for ICS leaders and improvement leads: Learning and Improving Across Systems; as well as our Primary-Secondary Interface Improvement Programme.
We must also acknowledge that the financial environment for all of our members is exceptionally challenging. As our recent report highlighted, a series of non-recurrent measures were taken in 2023/24, many of which will not be available in 2024/25. There is also a challenging paradox in relation to workforce numbers: the NHS Long Term Workforce Plan describes the need to expand the NHS workforce, but financial requirements are driving plans with freezes on workforce numbers, or significant reductions. We will continue to make the case that a clearer and more careful narrative at national and regional level is needed to guide discussions regarding financial plans and workforce numbers, and which balances financial responsibilities (including assurance of financial controls) with the transition to what is envisaged by the long-term workforce plan alongside the safety and quality responsibilities being managed by our members.
The operating context
The guidance recognises progress has been made and the challenging conditions that 2024/25 will bring. We particularly welcome the focus and acknowledgement of pressures on mental health services. Systems are required to include patients with mental health needs and children and young people in service recovery plans, and develop local plans to reduce long waits for and community and UEC mental health services.
It is positive that NHSE acknowledges that many of the targets contained in the guidance are ‘stretching’. We therefore believe that plans should be kept under regular review to consider the evolving operating and financial environment. Increasing the performance target on four-hour waits from 76 per cent to 78 per cent by March 2025 feels particularly challenging, especially without access to additional capital funding in this financial year, and given the 76 per cent target has not been met during any month of 2023/24 so far. Similarly, maintaining the target of 95 per cent of diagnostic tests to be delivered within six weeks by the same date will be difficult given the most recent data shows in January 2024 only 74 per cent of patients waited less than six weeks.
There are significant barriers standing in the way of the NHS making further progress over the next year – not least industrial action which, if left unresolved, will continue to cause operational instability and risk harm to patients. On primary care, it is welcome to see no new targets, but a continuation of those commitments already published through the Primary Care Access Recovery plan. However, in light of the proposed contract settlement for 2024/25 and an increasingly tight financial context, the opportunity to do more in primary care is limited without additional investment.
There are some fundamental issues the government must address to give the NHS the best chance to recover elective care and enable systems to drive overall improvements in the population’s health
It is unclear on the face of the guidance how organisations and systems will be supported to recover and make inroads against the targets listed in the guidance, as well as locally defined priorities. There are some fundamental issues the government must address to give the NHS the best chance to recover elective care and enable systems to drive overall improvements in the population’s health. These begin with ending the industrial dispute that continues to impede progress on waiting lists, finding the capital funding to deal with our crumbling estate and maintenance backlog and increasing capacity in social care so that fewer patients are left in hospital when they should be cared for closer to or in their homes.
In terms of system planning requirements, it is positive to see an emphasis on the role of the voluntary, community and social enterprise sector in supporting delivery of system priorities via an ask for ICBs develop a plan for working with the sector to drive transformation. More generally, while it is encouraging that NHSE has offered ICSs support in developing updated Joint Forward Plans (JFPs), the three-month turnaround for ICSs to refresh their JFPs is tight, especially given the capacity and financial pressures organisations at neighbourhood and place level are under.
NHSE has confirmed it will shortly engage with systems on a new oversight framework with the aim of providing further clarity on the role of NHSE and ICBs in oversight and ways of working with providers. The NHS Confederation will support this process to help ensure oversight incentivises integration as well as service recovery.
Finances
The single biggest contribution - at least £1.5 billion - to last year’s system deficit was the ongoing industrial action. While it is not within the gift of NHSE to address this particular issue, there is little consideration for how further action might affect the objectives or what process will be put in place to reassess these metrics throughout the year. The guidance states that the NHS aims to end the financial year in a net-zero financial position. While an understandable goal, this fails to heed recent history – and the ongoing industrial action – in which financial planning rounds have had to be consistently revisited owing to both highly ambitious expectations from the centre on ICS leaders, and various unpredictable events. The challenged financial position of key ICS partners, notably local government, will all be a barrier to progress, especially in relation to social care and public health.
It is worth noting that the planned increase in capital spending for the NHS, as announced in the 2024 Spring Budget, will not be seen until the next financial year and only relates to technology and data. Although we look forward to systems leading work to make best use of the investment to bolster recovery and improve services for patients, we also know the service faces a maintenance backlog of over £10 billion, which will be a significant barrier to achieving the ambitions set out.
Although ringfencing of funding is generally not conducive to support longer-term planning, we support this in the case of NHS dentistry budgets for 2024/25
Although ringfencing of funding is generally not conducive to support longer-term planning, we support this in the case of NHS dentistry budgets for 2024/25 given the dire state of provision, which is something our members are especially concerned about. In line with aims of ICSs on reducing health inequalities and improving population health outcomes, the focus within the planning guidance on vaccination programmes for children and adults is welcomed and will be enhanced by implementation of the vaccination strategy.
The continuation of the Mental Health Investment Standard is positive. However, given the tight financial envelope in 2024/25, mental health providers are concerned about the reality of this commitment. An additional £70 million of Service Development Funding, of which part will support increase children and young people’s access to services, is also welcome as this is a key area of pressure.
Incentivising productivity
The Chancellor announced the intention to set new productivity measures alongside the £3.4 billion productivity plan for the NHS in the Spring Budget. The planning guidance confirms that NHSE will report on productivity metrics at a national, ICB and trust level starting from the second half of the year, in line with the government’s productivity plan. We will work to support development of these metrics but speculate there is a chance of delay until after a general election, given their politically sensitive nature.
Where ICBs are asked to report on how well trusts are improving the primary–secondary care interface, NHSE should consider how to make these reporting processes as efficient and meaningful as possible
NHSE’s work to give a clearer picture of how productivity might be judged should be done in close cooperation with leaders who have the best understanding of their populations as well as the opportunities and levers available, in particular in developing new metrics for primary, community and mental health services. Where ICBs are asked to report on how well trusts are improving the primary–secondary care interface, NHSE should consider how to make these reporting processes as efficient and meaningful as possible to maximise staff time.
While we support the focus on productivity and recovering A&E performance, there is a risk within this incentive structure that focus is drawn away from some of the important actions outlined around increasing primary and community care capacity and reducing health inequalities that will support the development of integrated pathways of care and improved health outcomes. In particular, targeting financial incentives (through additional capital) at those trusts delivering over 80 per cent performance on A&E four-hour waits, as well as the most improving trusts, does not reward all parts of the system that collectively hold the levers needed to address what is a system-wide problem.
Key actions for members
ICBs and their partner and foundation trusts are asked to work with wider system partners to develop integrated system plans to meet the national objectives set out in the guidance alongside local priorities agreed by ICSs and signed off by ICB and trust boards. Requirements for plan submission are set out separately.
ICBs and their partner trusts are required to publish and share their JFPs with NHSE, integrated care partnerships and health and wellbeing boards by 30 June 2024. Guidance can be found on NHSE’s website.
Systems are asked work together to develop long-term infrastructure strategies, which will underpin JFPs and provide a system-level view of priorities for estates and capital investment by the end of July 2024. Guidance and resources can be found on NHSE’s website.
Members should also review the updated set of supplementary documents, which accompany the planning guidance.
How we will be supporting members
We will continue to engage with NHSE on behalf of members to represent their views and the reality of delivering services in the current environment. This includes continuing to advocate for further guidance and support on the areas not covered and call for greater recognition of the issues highlighted in our analysis, such as industrial action, productivity ambitions and funding.
We will also continue to support members with the implementation of guidance through our networks and forums, at every level across the system and our support offer for ICS leaders and improvement leads through the Learning and Improving Across Systems programme.
As one of our central asks of government, we will be focusing specifically on ensuring appropriate funding for the service over the next year. Building on our recent report on capital funding requirements, Investing to Save, we are assembling a member working group to test ideas for how the government might fund this ask and what innovative solutions we can offer. We invite any interested member to get in touch.



